Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Patients with Cardiovascular Disease
Heart Failure
HEART FAILURE
An increasing number of patients present
for sur-gery with either systolic and/or diastolic heart failure. Congestive
heart failure affects more than 5 million Americans. Heart failure may be
second-ary to ischemia, valvular heart disease, infectious agents, and many
types of cardiomyopathy. Most patients seek medical attention secondary to
heart failure because of complaints of dyspnea and fatigue. Heart failure develops
over time, as symptoms worsen (Figure 21–5). Patients generally undergo
echocardiography to diagnose structural heart defects, to detect signs of
cardiac “remodeling”, to determine the left ventricular ejection fraction, and
to assess the heart’s diastolic function. Laboratory evaluations of
concentration of brain natriuretic peptide (BNP) are likewise obtained to
distinguish heart failure from other causes of dyspnea. BNP is released from
the heart, and its elevation is associ-ated with impaired ventricular
function.In response to ventricular failure, the body attempts to compensate
for LV systolic function through the sympathetic and renin–angiotensin–
aldosterone system. Consequently, patients experi-ence salt retention, volume
expansion, sympathetic stimulation, and vasoconstriction. The heart dilates to
maintain the stroke volume in spite of decreased contractility. Over time,
compensatory mecha-nisms fail and contribute to the symptoms asso-ciated with
heart failure (eg, edema, tachycardia, decreased tissue perfusion). Patients
with systolic heart failure are likely to present to surgery hav-ing been
previously treated with diuretics, ACE inhibitors, angiotensin receptor
blockers, and
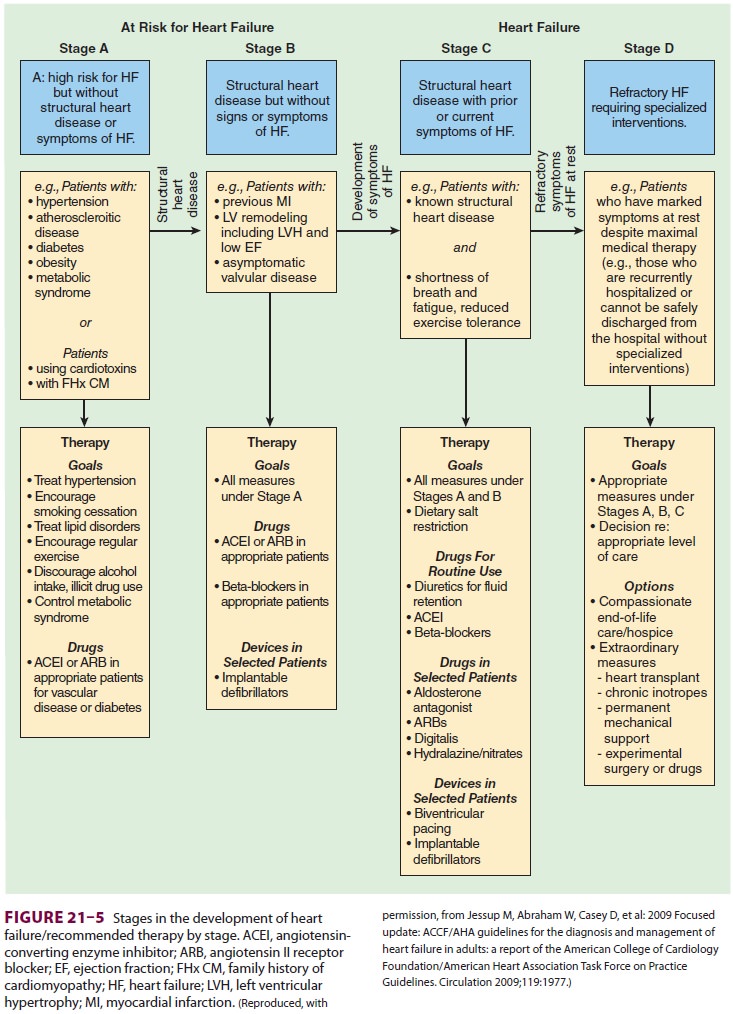
possibly aldosterone antagonists.
Electrolytes must be measured, as heart failure therapies frequently lead to
changes in serum potassium concentration. Angiotensin receptor blocker or ACE
inhibitor use may contribute to periinduction hypotension in the patient with
heart failure. ACE inhibitors are rarely associated with angioedema requiring
emergent airway management.
Diastolic ventricular dysfunction
pro-duces symptoms of congestion and heart failure. Myocardial relaxation is a
dynamic, not passive, process. The heart with preserved diastolic func-tion
accommodates volume during diastole, with minimal increases in left ventricular
end-diastolic pressure. Conversely, the heart with diastolic dys-function
relaxes poorly and produces increased left ventricular end-diastolic pressure.
The left ven-tricular end-diastolic pressure is transmitted to the left atrium
and pulmonary vasculature resulting in symptoms of congestion.
Anesthetic management of the patient
with heart failure requires careful assessment and opti-mization of
intravascular fluid volume—especially if positive inotropic agents,
vasoconstrictors, or vasodilators are used. In particular, patients with
diastolic dysfunction may tolerate increases in volume poorly, leading to
pulmonary congestion.
Related Topics