Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Patients with Cardiovascular Disease
Ischemic Heart Disease: Monitoring
MONITORING
Intraarterial pressure monitoring is
reasonable for all patients with severe CAD and major or multiple cardiac risk
factors who are undergoing any but the most minor procedures. Central venous
(or rarely pulmonary artery) pressure can be monitored during prolonged or
complicated procedures involv-ing large fluid shifts or blood loss. Less
invasive methods of cardiac output determination and vol-ume assessment have
been previously discussed in this text. Transesophageal echocardiography (TEE)
and transthoracic echocardiography (TTE) can provide valuable information, both
qualitative and quantitative, on contractility and ventricular cham-ber size
(preload) perioperatively. Intensive care unit staff increasingly use
ultrasound to assist in hemo-dynamic management. Numerous “basic” courses in
TEE and TTE are available to assist practitioners in performing “hemodynamic,”
as opposed to cardiac diagnostic TEE.Intraoperative detection of ischemia
depends on recognition of electrocardiographic changes, hemodynamic
manifestations, or regional wall motion abnormalities on TEE. Doppler TEE also
allows detection of the onset of mitral regurgitation caused by ischemic
papillary muscle dysfunction.
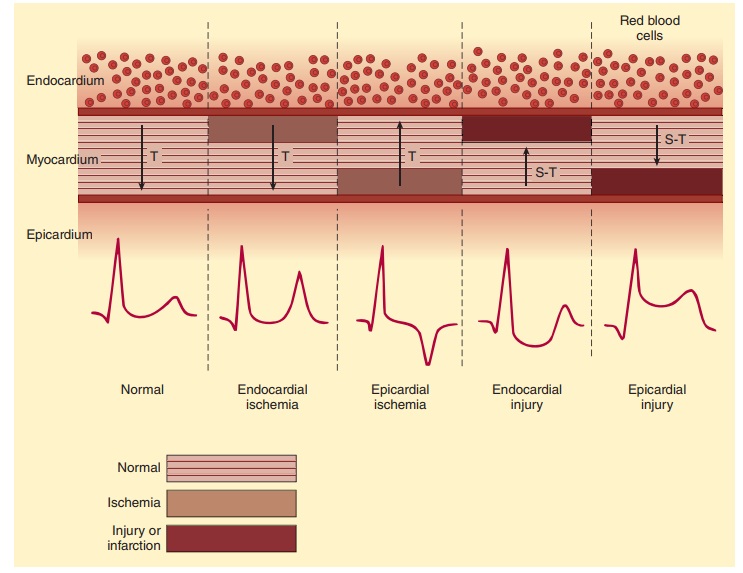
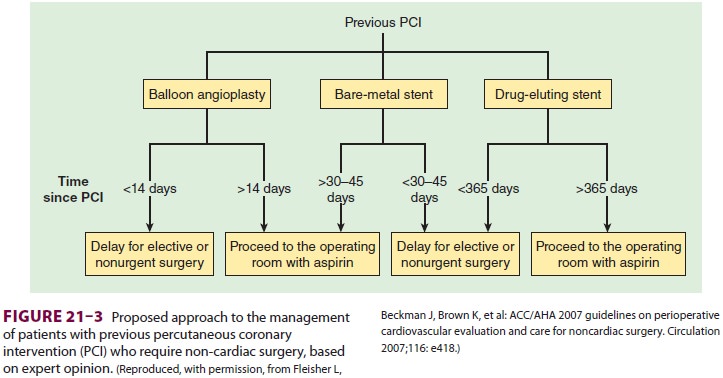
A. Electrocardiography
Early ischemic changes are subtle and
can often be overlooked. They involve changes in T-wave morphology, including
inversion, tenting, or both (Figure 21–1). More obvious ischemia may be
seen in the form of progressive ST-segment depression. Down-sloping and
horizontal ST depressions are of greater specificity for ischemia than is
up-sloping depression. New ST-segment elevations are rare dur-ing noncardiac
surgery and are indicative of severe ischemia, vasospasm, or infarction.
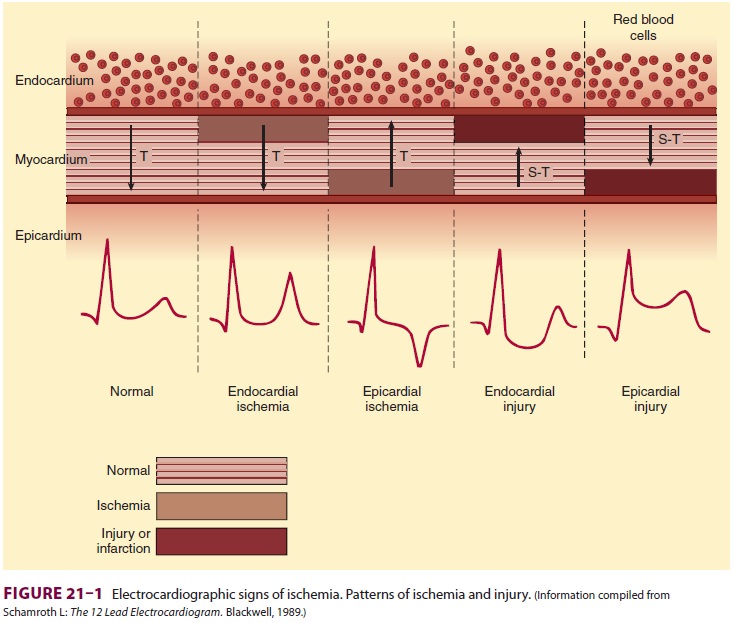
However, the increasing number of individuals treated with drug-eluting stents
can be problematic perioperatively, especially if surgical concerns necessitate
discontinu-ation of antiplatelet therapy (eg, emergency spine surgery). Such
patients are at very increased risk of thrombosis and perioperative MI.
Anesthesia staff should never for nonsurgical reasons (eg, desire to perform a
spinal anesthetic) discontinue antiplatelet or anti thrombotic agents
perioperatively without first discussing the risks and benefits of the
pro-posed anesthetic requiring suspension of antiplatelet therapy with the
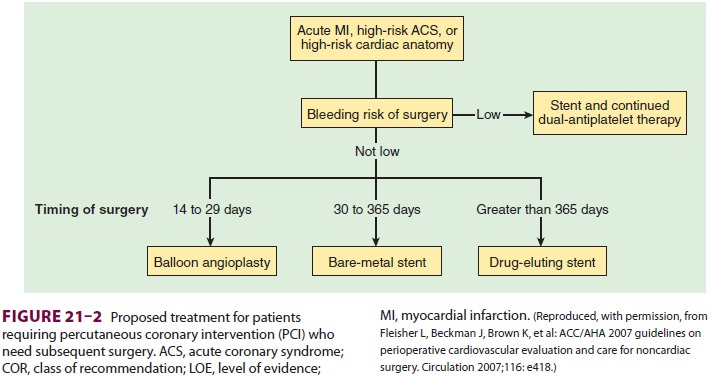
patient and his or her cardiologist. ACC/AHA offers recommendations on the
approach of bringing patients to surgery following percutane-ous coronary
interventions and the type of interven-tions suggested when subsequent surgery
is expected (Figures
21–2 and 21–3). It should be noted that an isolated
minor ST elevation in the mid-precordial leads (V3
and V4) can be a normal variant in young
patients. Ischemia may also present as an unexplained intraoperative atrial or
ventricular arrhythmia or the onset of a new conduction abnormality. The
sensitiv-ity of the ECG in detecting ischemia is related to the number of leads
monitored. Studies suggest that the V5,
V4, II, V2,
and V3 leads (in decreasing sensitivity) are
most useful. Ideally, at least two leads should be monitored simultaneously.
Usually, lead II is moni-tored for inferior wall ischemia and arrhythmias, and
V5 is monitored for anterior wall
ischemia. When only one channel can be monitored, a modified V5 lead provides the highest sensitivity.
B. Hemodynamic Monitoring
The most common hemodynamic
abnormalities observed during ischemic episodes are hyperten-sion and
tachycardia. They are almost always a cause (rather than the result) of
ischemia. Hypotension is a late and ominous manifestation of progressive
ventricular dysfunction. TEE readily will demon-strate a dysfunctional
ventricle and ventricular wall motion changes associated with myocardial
ischemia. Ischemia is frequently, but not always, associated with an abrupt
increase in pulmonary capillary wedge pres-sure. The sudden appearance of a
prominent v wave on the wedge
waveform is usually indicative of acute mitral regurgitation from ischemic
papillary muscle dysfunction or acute left ventricular dilatation.
C. Transesophageal Echocardiography
TEE can be helpful in detecting global and regional cardiac dysfunction, as well as valvular function in selected patients. Moreover, detection of new regional wall motion abnormalities is a rapid and more sensitive indicator of myocardial ischemia than the ECG. In animal studies in which coro-nary blood flow is gradually reduced, regional wall motion abnormalities develop before the ECG changes. Although the occurrence of new intraop-erative abnormalities correlates with postoperative MIs in some studies, not all such abnormalities are necessarily ischemic. Both regional and global abnormalities can be caused by changes in heart rate, altered conduction, preload, afterload, or drug-induced changes in contractility. Decreased systolic wall thickening may be a more reliable index for ischemia than endocardial wall motion alone.
Related Topics