Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Patients with Cardiovascular Disease
Hypertension:Preoperative Management
PREOPERATIVE MANAGEMENT
A recurring question in anesthetic
practice is the degree of preoperative hypertension that is accept-able for
patients scheduled for elective surgery. Except for optimally controlled
patients, most hyper-tensive patients present to the operating room with some
degree of hypertension. Although data suggest that even moderate preoperative
hypertension (dia-stolic pressure <90–110 mm Hg) is not clearly
statis-tically associated with postoperative
complications, other data indicate that the untreated or poorly con-trolled
hypertensive patient is more apt to experi-ence intraoperative episodes of myocardial ischemia, arrhythmias, or
both hypertension and hypotension. Intraoperative adjustments in anesthetic
depth and use of vasoactive drugs should reduce the incidence of postoperative
complications referable to poor preoperative control of hypertension.
Although patients should ideally undergo elective surgery only when rendered normoten-sive, this is not always feasible or necessarily desir-able because of altered cerebral autoregulation. Excessive reductions in blood pressure can com-promise cerebral perfusion. Moreover, the deci-sion to delay or to proceed with surgery should be individualized, based on the severity of the preop-erative blood pressure elevation; the likelihood of coexisting myocardial ischemia, ventricular dys-function, or cerebrovascular or renal complica-tions; and the surgical procedure (whether major surgically induced changes in cardiac preload or afterload are anticipated). With rare exceptions, antihypertensive drug therapy should be con-tinued up to the time of surgery. Some clinicians withhold ACE inhibitors and ARBs on the morn-ing of surgery because of their association with an increased incidence of intraoperative hypoten-sion; however, withholding these agents increases the risk of marked perioperative hypertension and the need for parenteral antihypertensive agents. It also requires the surgical team to remember torestart the medication after surgery. The decision to delay elective surgical procedures in patients with sustained preoperative diastolic blood pressures higher than 110 mm Hg should be made when the perceived benefits of delayed surgery exceed the risks. Unfortunately, there are few appropriate studies to guide the decision-making.
History
The preoperative history should inquire
into the severity and duration of the hypertension, the
drug therapy currently prescribed, and
the pres-ence or absence of hypertensive complications. Symptoms of myocardial
ischemia, ventricular failure, impaired cerebral perfusion, or peripheral
vascular disease should be elicited, as well as the patient’s record of
compliance with the drug regi-men. The patient should be questioned regarding
chest pain, exercise tolerance, shortness of breath (particularly at night),
dependent edema, postural lightheadedness, syncope, episodic visual
dis-turbances or episodic neurologic symptoms, and claudication. Adverse
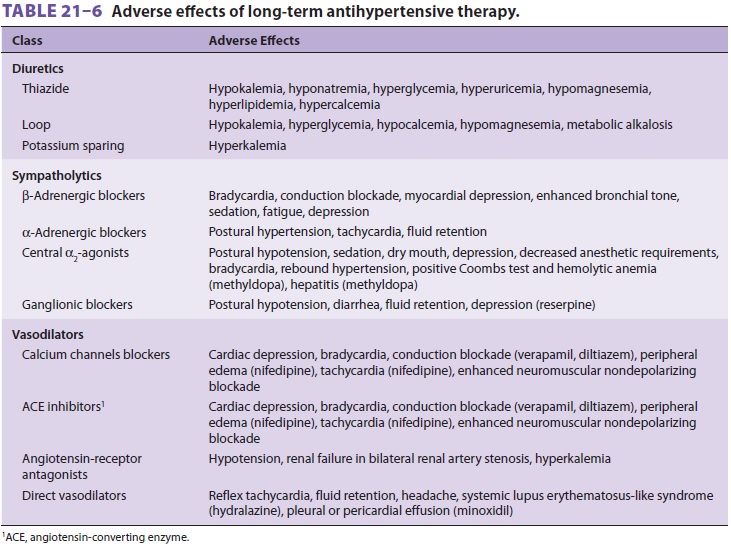
effects of current antihyper-tensive drug therapy (Table 21–6) should also be
identified.
Physical Examination & Laboratory Evaluation
Ophthalmoscopy is useful in hypertensive patients. Visible changes in the retinal vasculature usually parallel the severity and progression of arterioscle-rosis and hypertensive damage in other organs. An S4 cardiac gallop is common in patients with LVH. Other physical findings, such as pulmonary rales and an S 3 cardiac gallop, are late findings and indi-cate congestive heart failure. Blood pressure can be measured in both the supine and standing positions. Orthostatic changes can be due to volume deple-tion, excessive vasodilatation, or sympatholytic drug therapy; preoperative fluid administration can pre-vent severe hypotension after induction of anesthe-sia in these patients. Although asymptomatic carotid bruits are usually hemodynamically insignificant, they may be reflective of atherosclerotic vascular disease that may affect the coronary circulation. When a bruit is detected, further workup should be guided by the urgency of the scheduled surgery and the likelihood that further investigations, if diag-nostic, would result in a change in therapy. Doppler studies of the carotid arteries can be used to define the extent of carotid disease.
The ECG is often normal, but in patients
with a long history of hypertension, it may show evi-dence of ischemia,
conduction abnormalities, an old infarction, or LVH or strain. A normal ECG
does not exclude CAD or LVH. Similarly, a normal heart size on a chest
radiograph does not exclude ventricular hypertrophy. Echocardiography is a
sensitive test of LVH and can be used to evaluate ventricular systolic and
diastolic functions in patients with symptoms of heart failure. Chest
radiographs are rarely useful in an asymptomatic patient, but may show a
boot-shaped heart (suggestive of LVH), frank cardiomeg-aly, or pulmonary
vascular congestion.
Renal function is best evaluated by
measure-ment of serum creatinine and blood urea nitro-gen levels. Serum
electrolyte levels (K) should be determined in patients taking diuretics or
digoxin or those with renal impairment. Mild to moder-ate hypokalemia (3–3.5
mEq/L) is often seen in patients taking diuretics, but does not have adverse
outcome effects. Potassium replacement should be undertaken only in patients
who are symptomatic or who are also taking digoxin. Hypomagnesemia is often
present and may be a cause of perioperative arrhythmias. Hyperkalemia may be
encountered in patients who are taking potassium-sparing diuretics or ACE
inhibitors, particularly those with impaired renal function.
Premedication
Premedication reduces preoperative
anxiety and is desirable in hypertensive patients. Mild to moderate
preoperative hypertension often resolves following administration of an agent
such as midazolam.
Related Topics