Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Patients with Cardiovascular Disease
Perioperative Cardiovascular Evaluation and Preparation for Noncardiac Surgery
Perioperative Cardiovascular Evaluation and Preparation for
Noncardiac Surgery
The prevalence of cardiovascular disease
increases progressively with advancing age. Moreover, the number of patients
over 65 years of age is expected to increase by 25% to 35% over the next two
decades. Cardiovascular complications account for 25% to 50% of deaths
following noncardiac surgery.Perioperative myocardial infarction (MI),
pul-monary edema, systolic and diastolic heart failure, arrhythmias, and
thromboembolism are the most common diagnoses in patients with preexisting
car-diovascular disease. The incidence of postoperative cardiogenic pulmonary
edema is approximately 2% in all patients over 40 years of age, but it is 6% in
patients with a history of heart failure and 16% in patients with poorly
compensated heart failure. The relatively high prevalence of cardiovascular
disorders in surgical patients has given rise to attempts to define cardiacrisk or the likelihood of
intraoperative or postopera-tive fatal or life-threatening cardiac
complications.
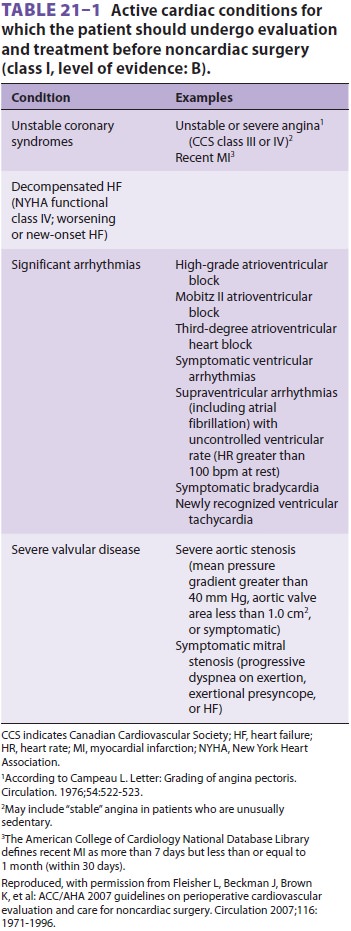
In 2007, the ACC/AHA Task Force Report
pro-duced revised guidelines for perioperative evaluation. The revised
guidelines stated that the patient’s medi-cal history is critical in
determining the requirements for preoperative cardiac evaluation and that
certain conditions (eg, unstable coronary syndromes and decompensated heart
failure) warrant cardiology intervention prior to all but emergency procedures
(Table 21–1).
The history should also review any past procedures, such as cardioverter
defibrillator implants, coronary stents, and other interventions.
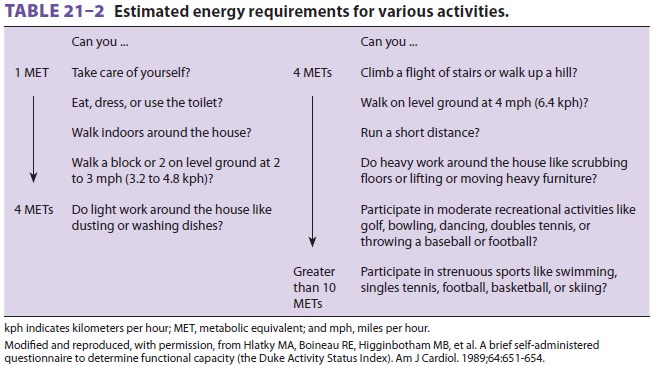
Additionally, the patient’s ability to
perform the tasks of daily living should be assessed as a guide to deter-mine
functional capacity. A patient with a history of cardiac disease and advanced
age, but good exercise tolerance, will likely have a lower perioperative risk
than a similar individual with dyspnea after minimal physical activity (Table 21–2).The
patient’s history should also seek signs of other disease processes that frequently
accom-pany heart disease. Cardiac patients often present with obstructive
pulmonary disease, reduced renal function, and diabetes mellitus.A physical
examination should be performed on all patients, and the heart and lungs should
be aus-cultated. The physical examination is especially use-ful in patients
with certain conditions. For example, if a murmur suggestive of aortic stenosis
is detected, additional ultrasound evaluation will likely be war-ranted, as
aortic stenosis substantially increases the risks in patients undergoing
noncardiac surgery.
The following conditions are associated
with increased risk:
·
Ischemic
heart disease (history of MI, evidence on electrocardiogram [ECG], chest pain)
·
Congestive
heart failure (dyspnea, pulmonary edema)
·
Cerebral
vascular disease (stroke)
·
High-risk
surgery (vascular, thoracic, abdominal, orthopedic)
·
Diabetes
mellitus
·
Preoperative
creatinine >2 mg/dL
Recent ACC/AHA guidelines identify
con-ditions that are a major cardiac risk and warrant intensive management prior
to all but emergent surgery. These conditions include: unstable coro-nary
syndromes (recent MI, unstable angina), decompensated heart failure,
significant arrhyth-mias, and severe valvular heart disease. The ACC/ AHA
guidelines identify an MI within 7 days, or one within 1 month with myocardium
at risk for ischemia, as “active” cardiac conditions. On the other hand,
evidence of past MI with no myocar-dium thought at ischemic risk is considered
a low risk for perioperative infarction after noncardiac surgery.
The ACC/AHA guidelines suggest a
stepwise approach to preoperative cardiac evaluation. Their recommendations are
classified as follows:
·
Class
I: Benefits >> risk
·
Class
IIa: Benefits >> risk, but scientific evidence
incomplete
·
Class
IIb: Benefits ≥ risk, and scientific evidence incomplete
·
Class
III: Risks >>benefits
Class I recommendations are as follows:
·
Patients
who have a need for emergency noncardiac surgery should proceed to the
operating room with perioperative surveillance and postoperative risk factor
management
·
Patients
with active cardiac conditions should be evaluated by a cardiologist and
treated according to ACC/AHA guidelines
·
Patients
undergoing low-risk procedures should proceed to surgery
·
Patients
with poor exercise tolerance (<4 metabolic
equivalents [METs]) and no known risk factors should proceed to surgery
Class IIa recommendations are as
follows:
·
Patients
with a functional capacity >4 METs and
without symptoms should proceed to surgery
·
Patients
with a functional capacity <4 METs or those
with an unknown functional capacity with three or more clinical risk factors
scheduled for vascular surgery should be tested, if management is likely to
change based on the results
·
Patients
with a functional capacity <4 METs or those
with an unknown functional capacity with three or more clinical risk factors
scheduled for intermediate-risk surgery should proceed to surgery with heart
rate control
·
Patients
with a functional capacity <4 METs or those
with an unknown functional capacity with one or two clinical risk factors who
are scheduled for vascular or intermediate-risk surgery should proceed to
surgery with heart rate control
The ACC/AHA guidelines also note, as
class IIb recommendations, that noninvasive testing might be considered if patient management changes in
patients with poor or unknown functional capacity or in patients undergoing
intermediate-risk surgery
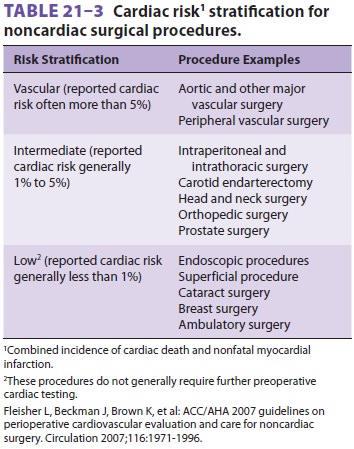
with three clinical risk factors.
Likewise, such test-ing might be indicated in patients with one or two clinical
risk factors scheduled for vascular or inter-mediate-risk surgery. Table 21–3
classifies surgical procedures according to risk.
The ACC/AHA guidelines also provide
specific recommendations regarding various conditions likely to be encountered
perioperatively.
Related Topics