Chapter: Medical Surgical Nursing: Management of Patients With Urinary Disorders
Urolithiasis
Urolithiasis
Urolithiasis
refers to stones (calculi) in the urinary tract. Stones are formed in the
urinary tract when urinary concentrations of substances such as calcium
oxalate, calcium phosphate, and uric acid increase. This is referred to as
supersaturation and is depen-dent on the amount of the substance, ionic
strength, and pH of the urine.
Pathophysiology
Stones
can also form when there is a deficiency of substances that normally prevent
crystallization in the urine, such as cit-rate, magnesium, nephrocalcin, and
uropontin. The fluid vol-ume status of the patient (stones tend to occur more
often in dehydrated patients) is another factor playing a key role in stone
development.
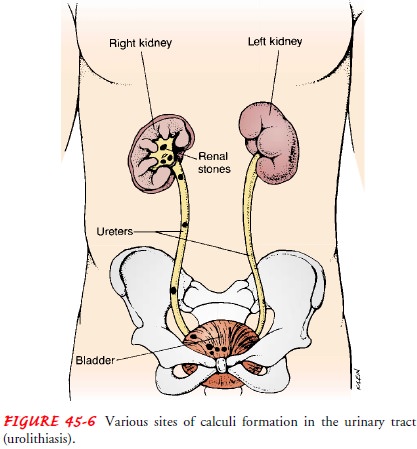
Calculi
may be found anywhere from the kidney to the blad-der. They vary in size from
minute granular deposits, called sand or gravel, to bladder stones as large as
an orange. The dif-ferent sites of calculi formation in the urinary tract are
shown in Figure 45-6.
Certain
factors favor the formation of stones, including in-fection, urinary stasis,
and periods of immobility (slows renal drainage and alters calcium metabolism).
In addition, increased calcium concentrations in blood and urine promote
precipita-tion of calcium and formation of stones (about 75% of all renal
stones are calcium-based). Causes of hypercalcemia (high serum calcium) and
hypercalciuria (high urine calcium) include the following:
· Hyperparathyroidism
· Renal tubular acidosis
· Cancers
· Granulomatous diseases
(sarcoidosis, tuberculosis), which may cause increased vitamin D production by
the granulo-matous tissue
· Excessive intake of
vitamin D
· Excessive intake of milk
and alkali
· Myeloproliferative
diseases (leukemia, polycythemia vera, multiple myeloma), which produce an
unusual prolifera-tion of blood cells from the bone marrow
For
patients with stones containing uric acid, struvite, or cys-tine, a thorough
physical examination and metabolic workup are indicated because of associated
disturbances contributing to the stone formation. Uric acid stones (5% to 10%
of all stones) may be seen in patients with gout or myeloproliferative
disorders. Struvite stones account for 15% of urinary calculi and form in
persistently alkaline, ammonia-rich urine caused by the presence of
urease-splitting bacteria such as Proteus,
Pseudomonas, Klebsiella, Staphy-lococcus, or Mycoplasma species. Predisposing factors for struvitestones
(commonly called infection stones) include neurogenic bladder, foreign bodies,
and recurrent UTIs. Cystine stones (1% to 2% of all stones) occur exclusively
in patients with a rare in-herited defect in renal absorption of cystine (an
amino acid).
Urinary
stone formation may also occur with inflammatory bowel disease and in patients
with an ileostomy or bowel resection because these patients absorb more
oxalate. Some medications that are known to cause stones in some patients
include antacids, acetazolamide (Diamox), vitamin D, laxatives, and high doses
of aspirin. In many patients, however, no cause may be found.
Urinary
stones account for about 328,000 hospital admissions each year. The occurrence
of urinary stones occurs predomi-nantly in the third to fifth decades of life
and affects men more than women. About half of patients with a single renal
stone have another episode within 5 years. Most stones contain calcium or
magnesium in combination with phosphorus or oxalate. Most stones are radiopaque
and can be detected by x-ray studies (Bihl & Meyers, 2001).
Clinical Manifestations
Signs
and symptoms of stones in the urinary tract depend on ob-struction, infection,
and edema. When the stones block the flow of urine, obstruction develops,
producing an increase in hydro-static pressure and distending the renal pelvis
and proximal ureter. Infection (pyelonephritis and cystitis with chills, fever,
and dysuria) can occur from constant irritation by the stone. Some stones cause
few, if any, symptoms while slowly destroying the functional units (nephrons)
of the kidney; others cause excruciating pain and discomfort.
Stones
in the renal pelvis may be associated with an intense, deep ache in the
costovertebral region. Hematuria is often present; pyuria may also be noted.
Pain originating in the renal area radiates anteriorly and downward toward the
bladder in the female and toward the testis in the male. If the pain suddenly
becomes acute, with tenderness over the costovertebral area, and nausea and
vom-iting appear, the patient is having an episode of renal colic. Diar-rhea
and abdominal discomfort may occur. These GI symptoms are due to renointestinal
reflexes and the anatomic proximity of the kidneys to the stomach, pancreas,
and large intestine.
Stones
lodged in the ureter (ureteral obstruction) cause acute, excruciating, colicky,
wavelike pain, radiating down the thigh and to the genitalia. Often, the
patient has a desire to void, but little urine is passed, and it usually
contains blood because of the abrasive action of the stone. This group of
symptoms is called ureteral colic. Colic is mediated by prostaglandin E, a
substance that increases ureteral contractility and renal blood flow and that
leads to increased intraureteral pressure and pain. In general, the patient
spontaneously passes stones 0.5 to 1 cm in diameter. Stones larger than 1 cm in
diameter usually must be removed or fragmented (broken up by lithotripsy) so
that they can be re-moved or passed spontaneously.
Stones
lodged in the bladder usually produce symptoms of irritation and may be
associated with UTI and hematuria. If the stone obstructs the bladder neck,
urinary retention occurs. If in-fection is associated with a stone, the
condition is far more serious, with sepsis threatening the patient’s life.
Assessment and Diagnostic Findings
The
diagnosis is confirmed by x-ray films of the kidneys, ureter, and bladder (KUB)
or by ultrasonography, intravenous urogra-phy, or retrograde pyelography. Blood
chemistries and a 24-hour urine test for measurement of calcium, uric acid,
creatinine, sodium, pH, and total volume are part of the diagnostic workup.
Dietary and medication histories and family history of renal stones are
obtained to identify factors predisposing the patient to the formation of
stones.
When
stones are recovered (stones may be freely passed by the patient or removed
through special procedures), chemical analy-sis is carried out to determine
their composition. Stone analysis can provide a clear indication of the
underlying disorder. For ex-ample, calcium oxalate or calcium phosphate stones
usually indi-cate disorders of oxalate or calcium metabolism, whereas urate
stones suggest a disturbance in uric acid metabolism.
Medical Management
The
basic goals of management are to eradicate the stone, to de-termine the stone
type, to prevent nephron destruction, to control infection, and to relieve any
obstruction that may be present. The immediate objective of treatment of renal
or ureteral colic is to re-lieve the pain until its cause can be eliminated.
Opioid analgesics are administered to prevent shock and syncope that may result
from the excruciating pain. NSAIDs may be as effective as other analgesics in
treating renal stone pain. They provide specific pain relief because they
inhibit the synthesis of prostaglandin E.
Hot
baths or moist heat to the flank areas may also be useful. Unless the patient
is vomiting or has heart failure or any other condition requiring fluid
restriction, fluids are encouraged. This increases the hydrostatic pressure
behind the stone, assisting it in its downward passage. A high, around-the-clock
fluid intake re-duces the concentration of urinary crystalloids, dilutes the
urine, and ensures a high urine output.
Nutritional
therapy plays an important role in preventing renal stones. Fluid intake is the
mainstay of most medical ther-apy for renal stones. Unless contraindicated, any
patient with renal stones should drink at least eight 8-ounce glasses of water
daily to keep the urine dilute. A urine output exceeding 2 L a day is advisable
(Chart 45-11).
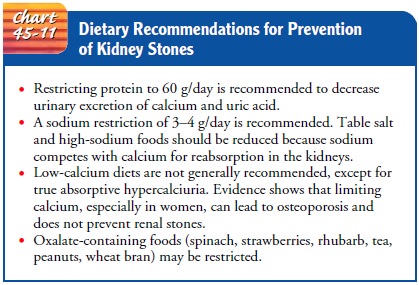
Calcium Stones. Historically,
patients with calcium-based renalstones were advised to restrict calcium in
their diet. Recent evi-dence, however, has questioned the advisability of this
practice, except for patients with type II absorptive hypercalciuria (half of
all patients with calcium stones), in whom stones are clearly due to excess
dietary calcium. Current research supports a liberal fluid intake along with
dietary restriction of protein and sodium. It is thought that a high-protein
diet is associated with increased uri-nary excretion of calcium and uric acid,
thereby causing a super-saturation of these substances in the urine. Similarly,
a high sodium intake has been shown in some studies to increase the amount of
calcium in the urine. The urine may be acidified by use of medications such as
ammonium chloride or acetohydrox-amic acid (Lithostat) (Trinchieri, Zanetti,
Curro & Lizzano, 2001; Williams, Child, Hudson et al., 2001).
Cellulose
sodium phosphate (Calcibind) may be effective in preventing calcium stones. It
binds calcium from food in the in-testinal tract, reducing the amount of
calcium absorbed into the circulation. If increased parathormone production
(resulting in increased serum calcium levels in blood and urine) is a factor in
the formation of stones, therapy with thiazide diuretics may be beneficial in
reducing the calcium loss in the urine and lowering the elevated parathormone
levels.
Uric Acid Stones. For uric
acid stones, the patient is placed on alow-purine diet to reduce the excretion
of uric acid in the urine. Foods high in purine (shellfish, anchovies,
asparagus, mushrooms, and organ meats) are avoided, and other proteins may be
limited. Allopurinol (Zyloprim) may be prescribed to reduce serum uric acid
levels and urinary uric acid excretion. The urine is alkalin-ized. For cystine
stones, a low-protein diet is prescribed, the urine is alkalinized, and
penicillamine is administered to reduce the amount of cystine in the urine.
Oxalate Stones. For oxalate
stones, a dilute urine is maintainedand the intake of oxalate is limited. Many
foods contain oxalate; however, only certain foods have been proved to increase
the urinary
excretion of oxalate significantly. These include spinach, strawberries,
rhubarb, chocolate, tea, peanuts, and wheat bran.
SURGICAL MANAGEMENT
If the
stone is not passed spontaneously or if complications occur, treatment
modalities may include surgical, endoscopic, or other procedures—for example,
ureteroscopy, extracorporeal shock wave lithotripsy (ESWL), or endourologic
(percutaneous) stone removal.
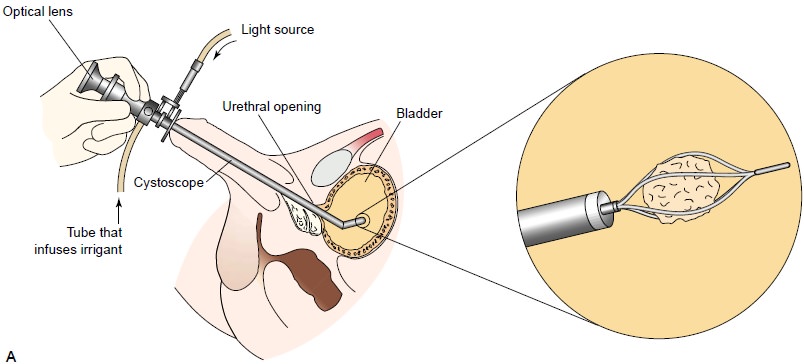
Ureteroscopy
(Fig. 45-7) involves first visualizing the stone and then destroying it. Access
to the stone is accomplished by in-serting a ureteroscope into the ureter and
then inserting a laser, electrohydraulic lithotriptor, or ultrasound device through
the ureteroscope to fragment and remove the stones. A stent may be inserted and
left in place for 48 hours or more after the procedure to keep the ureter
patent. Hospital stays are generally brief, and some patients can be treated as
outpatients.
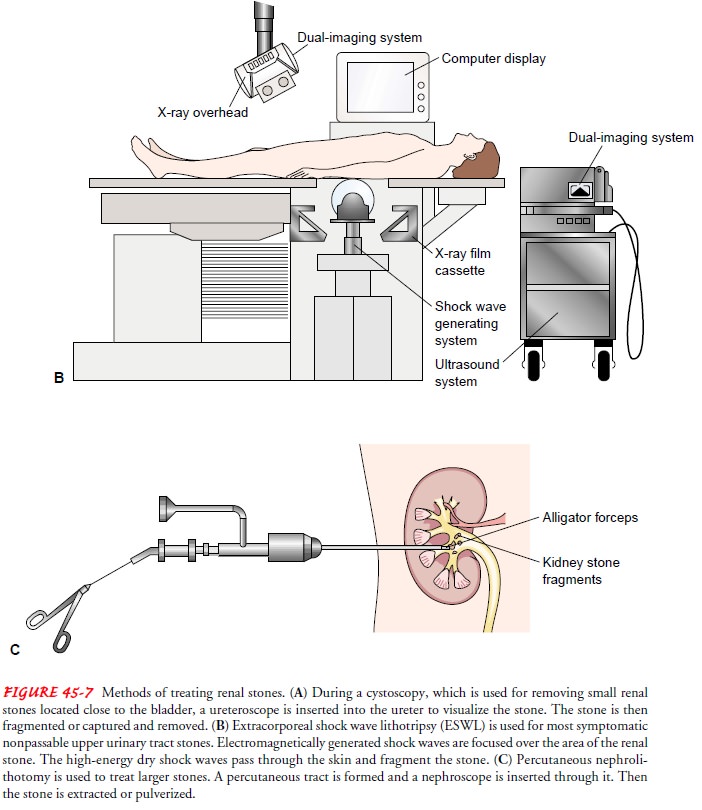
ESWL
is a noninvasive procedure used to break up stones in the calyx of the kidney
(see Fig. 45-7B). After the stones
are frag-mented to the size of grains of sand, the remnants of the stones are
spontaneously voided. In ESWL, a high-energy amplitude of pressure, or shock
wave, is generated by the abrupt release of en-ergy and transmitted through
water and soft tissues. When the shock wave encounters a substance of different
intensity (a renal stone), a compression wave causes the surface of the stone
to frag-ment. Repeated shock waves focused on the stone eventually re-duce it
to many small pieces. These small pieces are excreted in the urine, usually
without difficulty.
The
need for anesthesia for the procedure depends on the type of lithotriptor used,
which determines the number and intensity of shock waves delivered. An average
treatment comprises between 1,000 and 3,000 shocks. The first-generation
lithotriptors required use of either regional or general anesthesia. Second-
and third-generation lithotriptors, many of which also employ ultrasound
guidance, require little to no anesthesia (Tombolini, Ruoppolo, Bellorofonte et
al., 2000).
Although
the shock waves usually do not damage other tissue, discomfort from the
multiple shocks may occur. The patient is observed for obstruction and
infection resulting from blockage of the urinary tract by stone fragments. All
urine is strained after the procedure; voided gravel or sand is sent to the
laboratory for chemical analysis. Several treatments may be necessary to ensure
disintegration of stones. Although lithotripsy is a costly treat-ment, the
length of hospital stay is decreased, as is expense, be-cause an invasive
surgical procedure to remove the renal stone is avoided.
Endourologic
methods of stone removal (see Fig. 45-7C
) may be used to extract renal calculi that cannot be removed by other
procedures. A percutaneous nephrostomy or a percutaneous neph-rolithotomy
(which are similar procedures) may be performed, and a nephroscope is
introduced through the dilated percuta-neous tract into the renal parenchyma.
Depending on its size, the stone may be extracted with forceps or by a stone
retrieval basket. Alternatively, an ultrasound probe may be introduced through
the nephrostomy tube. Then, ultrasonic waves are used to pul-verize the stone.
Small stone fragments and stone dust are irri-gated and suctioned out of the
collecting system. Larger stones may be further reduced by ultrasonic
disintegration and then re-moved with forceps or a stone retrieval basket (Streem,
2000).
Electrohydraulic lithotripsy is a similar method in which an electrical discharge is used to create a hydraulic shock wave to break up the stone. A probe is passed through the cystoscope, and the
tip of the lithotriptor is placed near the stone. The strength of the discharge
and pulse frequency can be varied. This proce-dure is performed under topical
anesthesia. After the stone is ex-tracted, the percutaneous nephrostomy tube is
left in place for a time to ensure that the ureter is not obstructed by edema
or blood clots. The most common complications are hemorrhage, infec-tion, and
urinary extravasation. After the tube is removed, the nephrostomy tract closes
spontaneously.
Chemolysis,
stone dissolution using infusions of chemical so-lutions (eg, alkylating
agents, acidifying agents) for the purpose of dissolving the stone, is an
alternative treatment sometimes used in patients who are at risk for
complications of other types of ther-apy, who refuse to undergo other methods,
or who have stones (struvite) that dissolve easily. A percutaneous nephrostomy
is per-formed, and the warm irrigating solution is allowed to flow
con-tinuously onto the stone. The irrigating solution exits the renal collecting
system by means of the ureter or the nephrostomy tube. The pressure inside the
renal pelvis is monitored during the procedure.
Several
of these treatment modalities may be used in combi-nation to ensure removal of
the stones (Bihl & Meyers, 2001; Joshi, Kumar & Timoney, 2001; Liou
& Streem, 2001).
Surgical
removal was the major mode of therapy before the ad-vent of lithotripsy. Today,
however, surgery is performed in only 1% to 2% of patients. Surgical
intervention is indicated if the stone does not respond to other forms of
treatment. It may also be performed to correct anatomic abnormalities within
the kid-ney to improve urinary drainage. If the stone is in the kidney, the
surgery performed may be a nephrolithotomy (incision into the kidney with removal
of the stone) or a nephrectomy, if the kid-ney is nonfunctional secondary to
infection or hydronephrosis. Stones in the kidney pelvis are removed by a
pyelolithotomy, those in the ureter by ureterolithotomy, and those in the
bladder by cystotomy. If the stone is in the bladder, an instrument may be
inserted through the urethra into the bladder, and the stone is crushed in the
jaws of this instrument. Such a procedure is called a cystolitholapaxy
(Maheshwari, Oswal & Bansal, 1999; Monga Oglevie, 2000; Streem, 2000).
Related Topics