Chapter: Medical Surgical Nursing: Management of Patients With Urinary Disorders
Nursing Process: The Patient With Lower Urinary Tract Infection
NURSING
PROCESS: THE PATIENT WITH LOWER URINARY TRACT INFECTION
Nursing
care of the patient with lower UTI focuses on treating the underlying infection
and preventing its recurrence.
Assessment
A
history of signs and symptoms related to UTI is obtained from the patient with
a suspected UTI. The presence of pain, fre-quency, urgency, and hesitancy and
changes in urine are assessed, documented, and reported. The patient’s usual
pattern of void-ing is assessed to detect factors that may predispose him or
her to UTI. Infrequent emptying of the bladder, the association of symptoms of
UTI with sexual intercourse, contraceptive prac-tices, and personal hygiene are
assessed. The patient’s knowledge about prescribed antimicrobial medications
and preventive health care measures is also assessed. Additionally, the urine
is assessed for volume, color, concentration, cloudiness, and odor, all of
which are altered by bacteria in the urinary tract.
Diagnosis
NURSING DIAGNOSES
Based
on the assessment data, the nursing diagnoses may include the following:
· Acute pain related to
inflammation and infection of the ure-thra, bladder, and other urinary tract
structures
·
Deficient knowledge related to factors predisposing
the pa-tient to infection and recurrence, detection and prevention of
recurrence, and pharmacologic therapy
COLLABORATIVE PROBLEMS/ POTENTIAL COMPLICATIONS
Based
on assessment data, the following complications may develop:
· Renal failure due to
extensive damage of kidney
· Sepsis
Planning and Goals
Major
goals for the patient may include relief of pain and dis-comfort; increased
knowledge of preventive measures and treat-ment modalities; and absence of
complications.
Nursing Interventions
RELIEVING PAIN
The
pain associated with UTI is quickly relieved once effective antimicrobial
therapy is initiated. Antispasmodic agents may also be useful in relieving
bladder irritability and pain. Aspirin and ap-plying heat to the perineum help
relieve pain and spasm. The pa-tient is encouraged to drink liberal amounts of
fluids (water is the best choice) to promote renal blood flow and to flush the
bacte-ria from the urinary tract. Urinary tract irritants (eg, coffee, tea,
citrus, spices, colas, alcohol) are avoided. Frequent voiding (every 2 to 3
hours) is encouraged to empty the bladder completely be-cause this can
significantly lower urine bacterial counts, reduce urinary stasis, and prevent
reinfection.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Early
recognition of UTI and prompt treatment are essential to prevent recurrent
infection and the possibility of complications, such as renal failure and
sepsis. The goal of treatment is to pre-vent infection from progressing and
causing permanent renal damage and renal failure. Thus, the patient must be taught
to recognize early signs and symptoms, to test for bacteriuria, and to initiate
treatment as prescribed. Appropriate antimicrobial ther-apy, liberal fluid
intake, frequent voiding, and hygienic measures are commonly prescribed for
managing UTI. The patient is in-structed to notify the physician if fatigue,
nausea, vomiting, or pruritus occurs. Periodic monitoring of renal function
(creatinine clearance, blood urea nitrogen [BUN], and serum creatinine levels)
may be indicated for patients with repeated UTIs. If ex-tensive renal damage
does occur, dialysis may be necessary.
Patients
with UTI, especially catheter-associated infection, are at increased risk for
Gram-negative sepsis. Indwelling catheters should be avoided if possible and
removed at the earliest oppor-tunity (Thees & Dreblow, 1999). If an
indwelling catheter is nec-essary, however, specific nursing interventions are
initiated to prevent infection. These include the following:
· Using strict aseptic
technique during insertion of the small-est catheter possible
· Securing the catheter
with tape to prevent movement
· Frequently inspecting
urine color, odor, and consistency
· Performing meticulous
daily perineal care with soap and water
· Maintaining a closed
system
· Using the catheter’s
port to obtain urine specimens
Careful
assessment of vital signs and level of consciousness may warn of impending
sepsis. Blood cultures that are positive for in-fection and elevated WBC counts
are reported to the physician. At the same time, appropriate antibiotic therapy
and increased fluid intake are prescribed (intravenous antibiotic therapy and
fluids may be required). Preventing sepsis is key because the mortality rate
for Gram-negative sepsis is significant, especially in elderly patients.
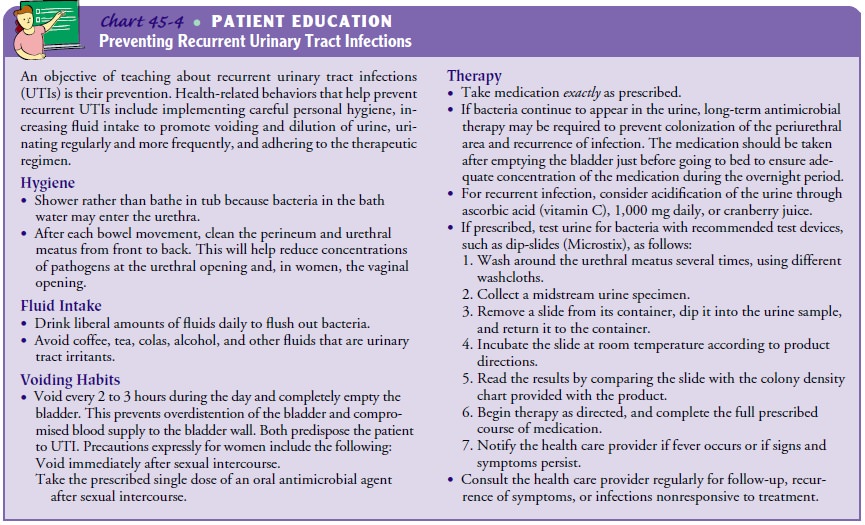
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
In
helping patients learn about and prevent or manage a recurrent UTI, the nurse
needs to implement teaching that meets individ-ual patient needs. For a
detailed discussion of patient teaching interventions, see Chart 45-4.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1) Experiences relief of
pain
a)
Reports absence of pain, urgency, dysuria, or
hesitancy on voiding
b)
Takes analgesic and antibiotic agents as prescribed
2) Explains UTIs and their
treatment
a)
Demonstrates knowledge of preventive measures and
prescribed treatments
b)
Drinks 8 to 10 glasses of fluids daily
c)
Voids every 2 to 3 hours
d)
Voids urine that is clear and odorless
3) Experiences no
complications
a)
Reports no symptoms of infection (fever, dysuria,
fre-quency) or renal failure (nausea, vomiting, fatigue, pruritus)
b)
Has normal BUN and serum creatinine levels,
negative urine and blood cultures
c)
Exhibits normal vital signs and temperature; no
signs or symptoms of sepsis
d)
Maintains adequate urine output more than 30 mL per
hour
Related Topics