Chapter: Medical Surgical Nursing: Management of Patients With Urinary Disorders
Nephrotic Syndrome - Primary Glomerular Diseases
NEPHROTIC
SYNDROME
Nephrotic syndrome is a primary glomerular disease
character-ized by the following:
· Marked increase in
protein in the urine (proteinuria)
· Decrease in albumin in
the blood (hypoalbuminemia)
· Edema
· High serum cholesterol
and low-density lipoproteins (hyper-lipidemia)
The
syndrome is apparent in any condition that seriously damages the glomerular
capillary membrane and results in in-creased glomerular permeability.
Pathophysiology
Nephrotic
syndrome can occur with almost any intrinsic renal disease or systemic disease
that affects the glomerulus. Although generally considered a disorder of
childhood, nephrotic syn-drome does occur in adults, including the elderly.
Causes include chronic glomerulonephritis, diabetes mellitus with
intercapillary glomerulosclerosis, amyloidosis of the kidney, systemic lupus
ery-thematosus, multiple myeloma, and renal vein thrombosis.
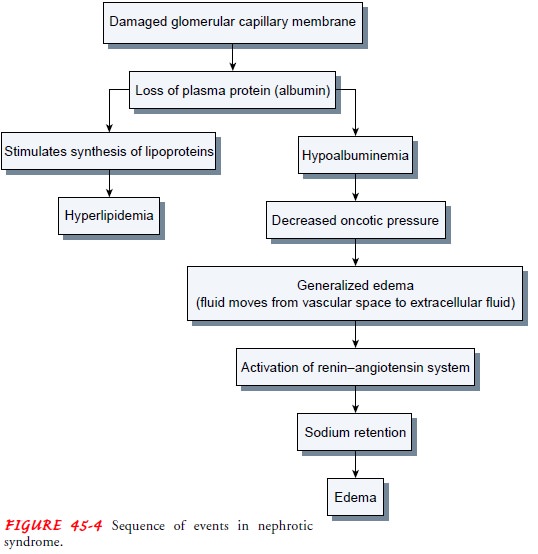
Nephrotic
syndrome is characterized by the loss of plasma protein, particularly albumin,
in the urine. Although the liver is capable of increasing the production of
albumin, it cannot keep up with the daily loss of albumin through the kidneys.
Thus, hypoalbuminemia results (Fig. 45-4).
Clinical Manifestations
The major manifestation of nephrotic syndrome is edema. It is usually soft and pitting and most commonly occurs around the eyes (periorbital), in dependent areas (sacrum, ankles, and hands), and in the abdomen (ascites). Other symptoms, including malaise, headache, irritability, and fatigue, are common (Fogo, 2000).
Assessment and Diagnostic Findings
Proteinuria
(predominately albumin) exceeding 3 to 3.5 g/day is sufficient for the
diagnosis of nephrotic syndrome. Protein elec-trophoresis and
immunoelectrophoresis may be performed on the urine to categorize the type of
proteinuria. The urine may also contain increased WBCs as well as granular and
epithelial casts. A needle biopsy of the kidney may be performed for histologic
examination of renal tissue to confirm the diagnosis. Recent stud-ies have
confirmed the usefulness of serum markers as a means of assessing the disease
process. Anti-C1q antibodies are the most reliable markers for assessing
disease activity in lupus nephritis (Moroni et al., 2001).
Complications
Complications
of nephrotic syndrome include infection (due to a deficient immune response),
thromboembolism (especially of the renal vein), pulmonary emboli, acute renal
failure (due to hypo-volemia), and accelerated atherosclerosis (due to
hyperlipidemia).
Medical Management
The
objective of management is to preserve renal function. Diuretic agents may be
prescribed for the patient with severe edema; how-ever, caution must be used
because of the risk of reducing the plasma volume to the point of impaired
circulation with subsequent prerenal acute renal failure. The use of
angiotensin-converting enzyme (ACE) inhibitors in combination with diuretics
often reduces the degree of proteinuria but may take 4 to 6 weeks to be
effective.
Other
medications used in treating nephrotic syndrome in-clude antineoplastic agents
(cyclophosphamide [Cytoxan]) or immunosuppressant medications (azathioprine
[Imuran], chlor-ambucil [Leukeran], or cyclosporine). It may be necessary to
re-peat treatment with corticosteroids if relapse occurs. Treatment of the
associated hyperlipidemia is controversial. The usual med-ications used to
treat hyperlipidemia are often ineffective or have serious consequences,
including muscle injury.
The
patient may be placed on a low-sodium, liberal-potassium diet to enhance the
sodium/potassium pump mechanism, thereby assisting in elimination of sodium to
reduce edema. Protein in-take should be about 0.8 g/kg/day, with emphasis on
high bio-logic proteins (dairy products, eggs, meats), and the diet should be
low in saturated fats (Deschenes & Doucet, 2000).
Nursing Management
In the
early stages of the disease, the nursing management is sim-ilar to that of the
patient with acute glomerulonephritis, but as the disease worsens, management
is similar to that of the patient with chronic renal failure (see the section
that follows). The pa-tient who is receiving corticosteroids or cyclosporine
requires in-structions about the medications and signs and symptoms that should
be reported to the physician. Dietary instructions may also be necessary.
Patients
with nephrotic syndrome need adequate instruction about the importance of
following all medication and dietary reg-imens so that their condition can
remain stable as long as possible. The patient must be made aware of the
importance of commu-nicating any health-related change to the health care
provider as soon as possible so that appropriate medication and dietary changes
can be made before further changes occur within the glomeruli. When indications
of an acute infection, such as an acute respiratory tract infection, are first
apparent, increased doses of maintenance corticosteroids have been found to
decrease the risk of relapse (Mattoo & Mahmoud, 2000).
Related Topics