Chapter: Medical Surgical Nursing: Management of Patients With Urinary Disorders
Continent Urinary Diversions
CONTINENT
URINARY DIVERSIONS
Continent Ileal Urinary Reservoir (Indiana Pouch)
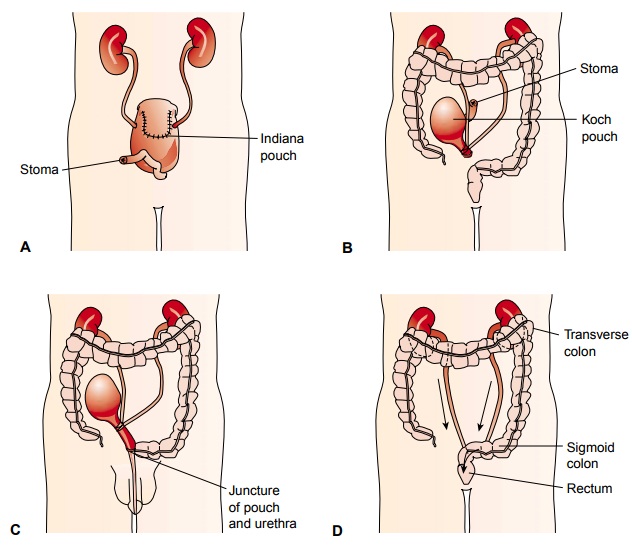
The
most common continent urinary diversion is the Indiana pouch, created for
patients whose bladder is removed or can no longer function (neurogenic
bladder). The Indiana pouch uses a segment of the ileum and cecum to form the
reservoir for urine (see Fig. 45-10A).
The ureters are tunneled through the muscu-lar bands of the intestinal pouch
and anastomosed. The reservoir is made continent by narrowing the efferent
portion of the ileum and sewing the terminal ileum to the subcutaneous tissue,
form-ing a continent stoma flush with the skin. The pouch is sewn to the
anterior abdominal wall around a cecostomy tube. Urine can collect in the pouch
until a catheter is inserted and the urine is drained.
The
pouch must be drained at regular intervals by a catheter to prevent absorption
of metabolic waste products from the urine, reflux of urine to the ureters, and
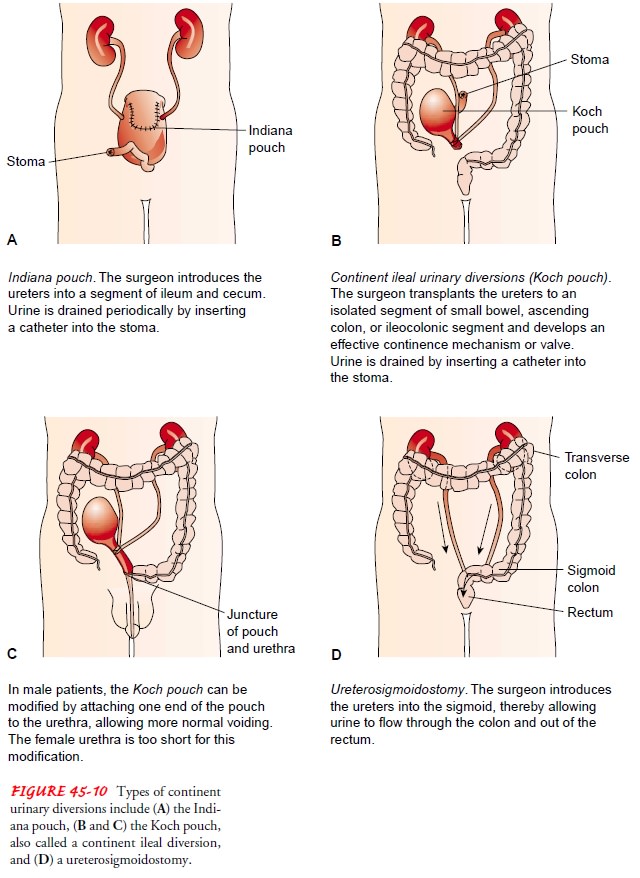
UTI. Postoperative nurs-ing care of the patient with a continent ileal urinary
pouch is sim-ilar to nursing care of the patient with an ileal conduit.
However, these patients usually have additional drainage tubes (cecostomy
catheter from the pouch, stoma catheter exiting from the stoma, ureteral
stents, Penrose drain, as well as a urethral catheter), as depicted in Figure
45-11. All drainage tubes must be carefully monitored for patency and amount
and type of drainage. The ce-costomy tube is irrigated two or three times daily
to remove mucus from the pouch and prevent blockage.
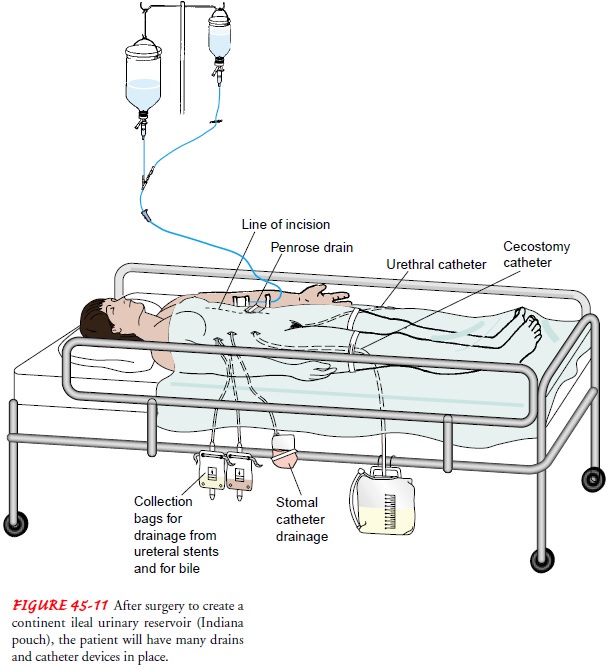
Other variations of continent urinary reservoirs include the Kock pouch (U-shaped pouch constructed of ileum, with a nipple-like one-way valve; see Fig. 45-10B and C ) and the Charleston pouch (uses the ileum and ascending colon as the pouch, with the appendix and colon junction serving as the one-way valve mech-anism). With both of these methods, the pouch must be drained at regular intervals by a catheter.
Ureterosigmoidostomy
Ureterosigmoidostomy, another form of continent urinary
di-version, is an implantation of the ureters into the sigmoid colon (see Fig.
45-10D). It is usually performed in
patients who have had extensive pelvic irradiation, previous small bowel
resection, or coexisting small bowel disease.
After
surgery, voiding occurs from the rectum (for life), and an adjustment in
lifestyle will be necessary because of urinary fre-quency (as often as every 2
hours). Drainage has a consistency equivalent to watery diarrhea, and the
patient has some degree of nocturia. Patients usually need to plan activities
around the fre-quent need to urinate, which in turn may affect the patient’s
so-cial life. Patients have the advantage, however, of urinary control without
having to wear an external appliance.
Nursing Management
In
addition to the usual preoperative regimen, the patient may be placed on a
liquid diet for several days preoperatively to reduce residue in the colon.
Antibiotic agents (neomycin, kanamycin) are administered to disinfect the
bowel. Ureterosigmoidostomy requires a competent anal sphincter, adequate renal
function, and active renal peristalsis. The degree of anal sphincter control
may be determined by assessing the patient’s ability to retain enemas.
The
postoperative regimen initially includes placing a catheter in the rectum to
drain the urine and prevent reflux of urine into the ureters and kidneys. The tube
is taped to the buttocks, and special skin care is given around the anus to
prevent excoriation. Irrigations of the rectal tube may be prescribed, but
force is never used because of the danger of introducing bacteria into the
newly implanted ureters.
MONITORING FLUID AND ELECTROLYTES
In
ureterosigmoidostomy, larger areas of the bowel mucosa are exposed to urine and
electrolyte reabsorption. As a result, elec-trolyte imbalance and acidosis may
occur. Potassium and mag-nesium in the urine may cause diarrhea. Fluid and
electrolyte balance is maintained in the immediate postoperative period by
closely monitoring the serum electrolyte levels and administering appropriate
intravenous infusions. Acidosis may be prevented by placing the patient on a
low-chloride diet supplemented with sodium potassium citrate.
The
patient should be instructed never to wait longer than 2 to 3 hours before
emptying urine from the intestine. This keeps rectal pressure low and minimizes
the absorption of urinary con-stituents from the colon. It is essential to
teach the patient about the symptoms of UTI: fever, flank pain, and frequency.
RETRAINING THE ANAL SPHINCTER
After
the rectal catheter is removed, the patient learns to control the anal
sphincter through special sphincter exercises. At first, uri-nation is
frequent. With reassurance and encouragement and the passage of time, the
patient gains greater control and learns to dif-ferentiate between the need to
void and the need to defecate.
PROMOTING DIETARY MEASURES
Specific
dietary instructions include avoidance of gas-forming foods (flatus can cause
stress incontinence and offensive odors). Other ways to avoid gas are to avoid
chewing gum, smoking, and any other activity that involves swallowing air. Salt
intake may be restricted to prevent hyperchloremic acidosis. Potassium intake
is increased through foods and medication because potassium may be lost in
acidosis.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Pyelonephritis
(upper UTI) due to reflux of bacteria from the colon is fairly common.
Long-term antibiotic therapy may be prescribed to prevent infection. A late
complication is adenocar-cinoma of the sigmoid colon, possibly from cellular
changes due to exposure of the colonic mucosa to urine.
Urinary
carcinogens promote late malignant transformation of the colon after a
ureterosigmoidostomy. Therefore, diligent patient teaching regarding the need
for life-long medical follow-up is essential (Guy et al, 2001; Huang &
McPherson, 2000).
Related Topics