Chapter: Medical Surgical Nursing: Management of Patients With Urinary Disorders
Cutaneous Urinary Diversions
CUTANEOUS
URINARY DIVERSIONS
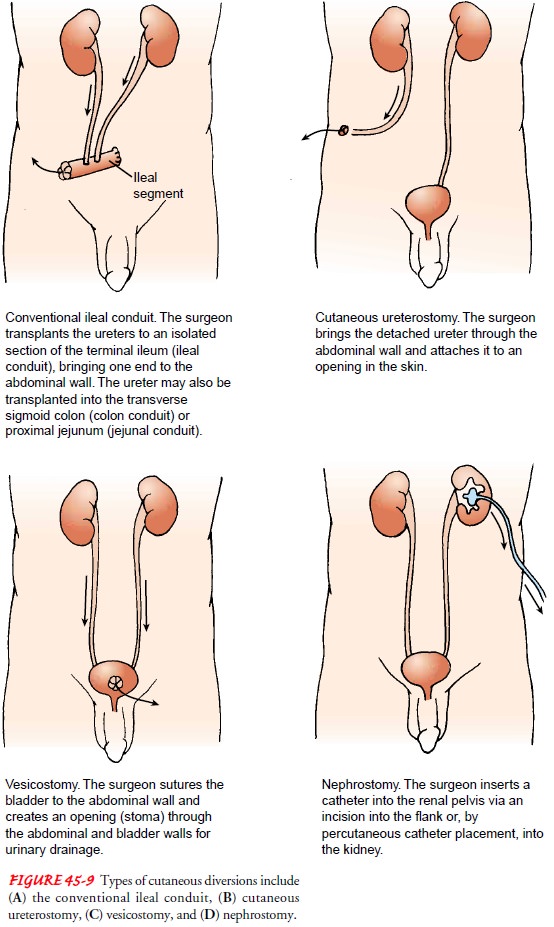
Ileal Conduit (Ileal Loop)
The ileal conduit, the oldest of the urinary diversion procedures, is considered the gold standard because of the low number of complications and surgeons’ familiarity with the procedure. In an ileal conduit, the urine is diverted by implanting the ureter into a
12-cm loop of ileum that is led out through the abdominal wall. This loop of
ileum is a simple conduit (passageway) for urine from the ureters to the
surface. A loop of the sigmoid colon may also be used. An ileostomy bag is used
to collect the urine. The resected (cut) ends of the remaining intestine are
anastomosed (connected) to provide an intact bowel.
Stents,
usually made of thin, pliable tubing, are placed in the ureters to prevent
occlusion secondary to postsurgical edema. The bilateral ureteral stents allow
urine to drain from the kidney to the stoma and provide a method for accurate
measurement of urine output. They may be left in place 10 to 21 days postopera-tively.
Jackson-Pratt tubes or other types of drains are inserted to prevent the
accumulation of fluid in the space created by removal of the bladder.
After
surgery, a skin barrier and a transparent, disposable uri-nary drainage bag are
applied around the conduit and connected to drainage. A custom-cut appliance is
used until the edema sub-sides and the stoma shrinks to normal size. The clear
bag allows the stoma to be seen and the patency of the stent and the urine
output to be monitored. The ileal bag drains urine constantly (not feces). The
appliance (bag) usually remains in place as long as it is watertight; it is
changed when necessary to prevent leak-age of urine.
Complications
that may follow placement of an ileal conduit include wound infection or wound
dehiscence, urinary leakage, ureteral obstruction, hyperchloremic acidosis,
small bowel ob-struction, ileus, and stomal gangrene. Delayed complications
in-clude ureteral obstruction, contraction or narrowing of the stoma (stomal
stenosis), renal deterioration due to chronic reflux, pyelo-nephritis, and
renal calculi.
Nursing Management
In the
immediate postoperative period, urine volumes are moni-tored hourly. An output
below 30 mL/h may indicate dehydration or an obstruction in the ileal conduit,
with possible backflow or leakage from the ureteroileal anastomosis. Throughout
the patient’s hospitalization, the nurse monitors closely for complications,
re-ports signs and symptoms of them promptly, and intervenes quickly to prevent
their progression.
PROMOTING URINE OUTPUT
A
catheter may be inserted through the urinary conduit if pre-scribed to monitor
the patient for possible stasis or residual urine from a constricted stoma.
Urine may drain through the bilateral ureteral stents as well as around the stents.
If the ureteral stents are not draining, the nurse may be instructed to
irrigate them with 5 to 10 mL of sterile normal saline solution. It is
important to avoid any tension on the stents because this may dislodge them.
Hematuria may be noted in the first 48 hours after surgery but usually resolves
spontaneously.
PROVIDING STOMA AND SKIN CARE
Because
the patient requires specialized care, a consultation is ini-tiated with an
enterostomal therapist or clinical nurse specialist in skin care. The stoma is
inspected frequently for color and viabil-ity. A healthy stoma is beefy red. A
change from this normal color to a dark purplish color suggests that the
vascular supply may be compromised. If cyanosis and a compromised blood supply
per-sist, surgical intervention may be necessary. The stoma is not sen-sitive
to touch, but the skin around the stoma becomes sensitive if urine or the
appliance irritates it. The skin is inspected for (1) signs of irritation and
bleeding of the stomal mucosa, (2) encrustation and skin irritation around the
stoma (from alkaline urine coming in contact with exposed skin), and (3) wound
infections.
TESTING URINE AND CARING FOR THE OSTOMY
Moisture
in bed linens or clothing or the odor of urine around the patient should alert
the nurse to the possibility of leakage from the appliance, potential
infection, or a problem in hygienic management. Because severe alkaline
encrustation can accumu-late rapidly around the stoma, the urine pH is kept
below 6.5 by administration of ascorbic acid by mouth. Urine pH can be
de-termined by testing the urine draining from the stoma, not from the
collecting appliance. A properly fitted appliance is essential to prevent
exposure of the peristomal skin (skin around the stoma) to urine. If the urine
is foul-smelling, the stoma is catheterized, if prescribed, to obtain a urine
specimen for culture and sensitivity testing.
ENCOURAGING FLUIDS AND RELIEVING ANXIETY
Because
mucous membrane is used in forming the conduit, the patient may excrete a large
amount of mucus mixed with urine. This causes many patients to feel anxious. To
help relieve this anxiety, the nurse reassures the patient that this is a
normal oc-currence after an ileal conduit procedure. The nurse encourages
adequate fluid intake to flush the ileal conduit and decrease the accumulation
of mucus.
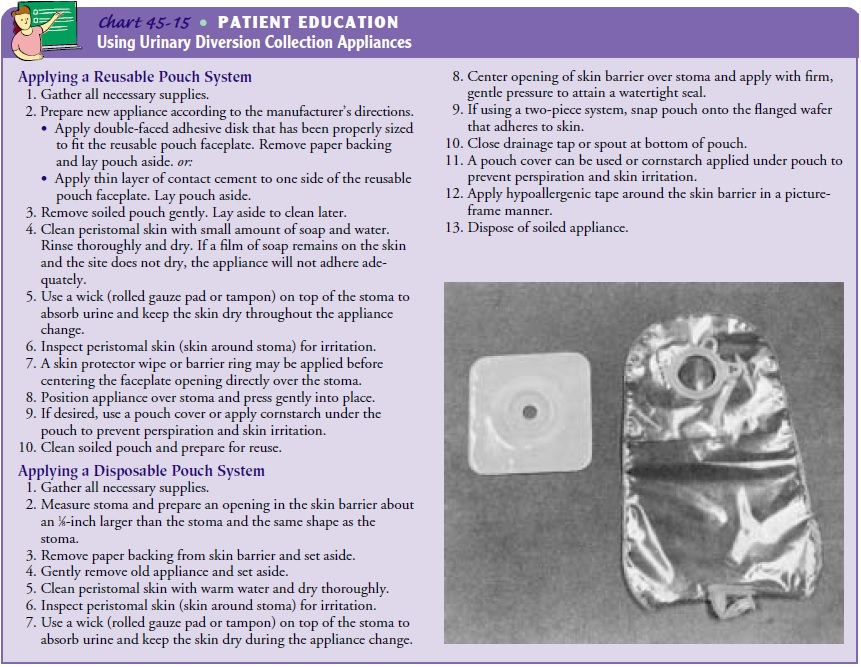
SELECTING THE OSTOMY APPLIANCE
Various
urine collection appliances are available, and the nurse is instrumental in
selecting an appropriate one. The urinary appli-ance may consist of one or two
pieces and may be disposable (usu-ally used once and discarded) or reusable.
The choice of appliance is determined by the location of the stoma and by the
patient’s normal activity, manual dexterity, visual function, body build,
economic resources, and preference.
A
reusable appliance has a faceplate that is attached to the skin surface with
cement or adhesive. Either reusable pouches or dis-posable pouches may be used
with the reusable faceplate. Dis-posable appliances have the advantages of
having a surface that is already prepared for application to the skin and of
being light-weight and easy to conceal. A skin barrier must be used to pro-tect
the skin from excoriation due to exposure to the urine.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care.
Patient
education begins in thehospital but continues into the home setting because
patients are usually discharged within days of surgery. The nurse teaches the
patient how to assess and manage the urinary diversion as well as how to deal
with body image changes. An enterostomal therapist is invaluable in consulting
with the nurse on various aspects of care and patient education.
Changing the Appliance.
The patient
and family are taught toapply and change the appliance so that they are comfortable
carry-ing out the procedure and can do so proficiently. Ideally, the appliance
system is changed before the system leaks and at a time that is convenient for
the patient. Many patients find early morn-ing most convenient because the
urine output is reduced. A vari-ety of appliances are available; an average
collecting appliance lasts 3 to 7 days before leakage occurs.
Regardless
of the type of appliance used, a skin barrier is es-sential to protect the skin
from irritation and excoriation. To maintain peristomal skin integrity, a skin
barrier or leaking pouch is never patched with tape to prevent accumulation of
urine under the skin barrier or faceplate. The patient is instructed to avoid
moisturizing soaps when cleaning the area because they in-terfere with the
adhesion of the pouch. Because the degree to which the stoma protrudes is not
the same in all patients, there are various accessories and custom-made
appliances to solve in-dividual problems. Guidelines for applying reusable and
dispos-able systems are presented in Chart 45-15.
Controlling Odor.
The patient
is instructed to avoid foods thatgive the urine a strong odor (eg, asparagus,
cheese, eggs). Today, most appliances contain odor barriers, but a few drops of
liquid deodorizer or diluted white vinegar may be introduced through the drain
spout into the bottom of the pouch with a syringe or eyedropper to reduce
odors. Ascorbic acid by mouth helps acid-ify the urine and suppress urine odor.
Patients should be cau-tioned about putting aspirin tablets in the pouch to
control odor because they may ulcerate the stoma. Also, the patient is
re-minded that odor will develop if the pouch is worn too long and not cared
for properly.
Managing the Ostomy Appliance.
The patient
is instructed toempty the pouch by means of a drain valve when it is one-third
full because the weight of the urine will cause the pouch to separate from the
skin if filled more. Some patients prefer wearing a leg bag attached with an
adapter to the drainage apparatus. To promote uninterrupted sleep, a collecting
bottle and tubing (one unit) are snapped onto an adapter that connects to the
ileal appliance. A small amount of urine is left in the bag when the adapter is
attached to prevent the bag from collapsing against itself. The tubing may be
threaded down the pajama or pants leg to prevent kinking. The collecting bottle
and tubing are rinsed daily with cool water and once a week with a 3:1 solution
of water and white vinegar.
Cleaning and Deodorizing the Appliance.
Usually, the reusable ap-pliance is rinsed in warm water and soaked in a 3 1 solution of water and white vinegar or a commercial deodorizing solution for 30
minutes. It is rinsed with tepid water and air-dried away from direct sunlight.
(Hot water and exposure to direct sunlight dry the pouch and increase the
incidence of cracking.) After drying, the appliance may be powdered with
cornstarch and stored. Two appliances are necessary—one to be worn while the
other is air-drying.
Continuing Care.
Follow-up
care is essential to determine howthe patient has adapted to the body image
changes and lifestyle changes. Referral for home care is indicated to determine
how well the patient and family are coping with the changes necessi-tated by
altered urinary drainage. The home care nurse assesses the patient’s physical
status and emotional response to urinary di-version. Additionally, the nurse
assesses the ability of the patient and family to manage the urinary diversion
and appliance, rein-forces previous teaching, and provides additional
information (eg, community resources, sources of ostomy supplies, insurance
coverage for supplies).
As the
postoperative edema subsides, the home care nurse as-sists in determining the
appropriate changes needed in the os-tomy appliance. The stoma opening is
recalibrated every 3 to 6 weeks for the first few months postoperatively. The
correct ap-pliance size is determined by measuring the widest part of the stoma
with a ruler. The permanent appliance should be no more than 1.6 mm (1⁄8 inch) larger than the
diameter of the stoma and the same shape as the stoma to prevent contact of the
skin with drainage.
The
nurse encourages the patient and family to contact the United Ostomy
Association and local ostomy association for vis-its, reassurance, and
practical information. In addition, the local division of the American Cancer
Society can provide medical equipment and supplies and other resources for the
patient who has undergone ostomy surgery for cancer.
The
home care nurse also assesses the patient for potential long-term
complications, such as ureteral obstruction, stomal stenosis, hernias, or
deterioration of renal function, and reinforces previous teaching about these
complications.
The
nurse also needs to remind the patient who has had surgery for carcinoma to
have a yearly physical examination and chest x-ray to assess for metastases.
Periodic evaluation of re-maining renal function (creatinine clearance, serum
BUN and creatinine levels) is also essential. Long-term monitoring for ane-mia
is performed to identify a vitamin B deficiency that may occur when a
significant portion of the terminal ileum is re-moved. This may take several
years to develop and can be treated with vitamin B injections. Additionally,
the patient is reminded of the importance of participating in health promotion
activities and recommended health screening.
Cutaneous Ureterostomy
A cutaneous ureterostomy (see Fig. 45-9),
in which the ureters are directed through the abdominal wall and attached to an
opening in the skin, is used for selected patients with ureteral obstruction
(advanced pelvic cancer); for poor-risk patients, be-cause it requires less
extensive surgery than other urinary diversion procedures; and for patients who
have had previous abdominal irradiation.
A
urinary appliance is fitted immediately after surgery. The management of the
patient with a cutaneous ureterostomy is sim-ilar to the care of the patient
with an ileal conduit, although the stomas are usually flush with the skin or
retracted.
Other Cutaneous Urinary Diversions
Other
cutaneous urinary diversions are used less frequently and are most often used
to bypass obstructions.
Related Topics