Chapter: Medical Surgical Nursing: Management of Patients With Urinary Disorders
Urinary Tract Cancers
Urinary Tract Cancers
The
American Cancer Society (2002) estimates increases in both the incidence and
death rates of all urinary tract cancers over pre-vious reports; however, while
the rate of estimated new cases of bladder cancer has increased, there has been
a slight decrease in the rate of new cases of kidney and renal pelvis cancer in
the last few years. Urinary tract cancers include those of the urinary
blad-der, kidney and renal pelvis, ureter, and other urinary structures, such
as the prostate. Tobacco use continues to be a leading cause of all urinary tract
cancers.
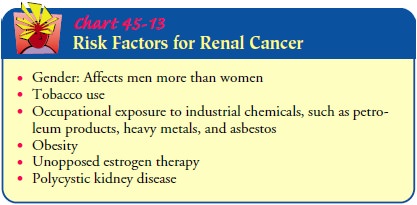
CANCER OF THE KIDNEY
Cancer
of the kidney accounts for about 3.7% of all cancers in adults in the United
States. It affects almost twice as many men as women. The most common type of
renal tumor is renal cell or renal adenocarcinoma, accounting for more than 85%
of all kid-ney tumors (Hock et al., 2002). These tumors may metastasize early
to the lungs, bone, liver, brain, and contralateral kidney. One third of
patients have metastatic disease at the time of diag-nosis. The incidence of
all stages of kidney cancer has increased
in the
last two decades in the United States. Although enhanced imaging techniques
account for improved detection of early-stage kidney cancer, it is unknown why
the rate of late-stage kidney cancers is higher (Hock, Lynch & Balaji,
2002) (Chart 45-13).
Clinical Manifestations
Many
renal tumors produce no symptoms and are discovered on a routine physical
examination as a palpable abdominal mass. The classic triad of signs and
symptoms, which occurs in only 10% of patients, comprises hematuria, pain, and
a mass in the flank. The usual sign that first calls attention to the tumor is
pain-less hematuria, which may be either intermittent and microscopic or
continuous and gross. There may be a dull pain in the back from the pressure
produced by compression of the ureter, exten-sion of the tumor into the
perirenal area, or hemorrhage into the kidney tissue. Colicky pains occur if a
clot or mass of tumor cells passes down the ureter. Symptoms from metastasis
may be the first manifestations of renal tumor and may include unexplained
weight loss, increasing weakness, and anemia.
Assessment and Diagnostic Findings
The
diagnosis of a renal tumor may require intravenous urography, cystoscopic
examination, nephrotomograms, renal angiograms, ultrasonography, or a CT scan.
These tests may be exhausting for patients already debilitated by the systemic
effects of a tumor as well as for elderly patients and those who are anxious
about the di-agnosis and outcome. The nurse assists the patient to prepare
physically and psychologically for these procedures and monitors carefully for
signs and symptoms of dehydration and exhaustion.
Medical Management
The
goal of management is to eradicate the tumor before metas-tasis occurs
(Kirkali, Tuzel & Munga, 2002).
SURGICAL MANAGEMENT
A
radical nephrectomy is the preferred treatment if the tumor can be removed.
This includes removal of the kidney (and tumor), adrenal gland, surrounding
perinephric fat and Gerota’s fascia, and lymph nodes. Radiation therapy,
hormonal therapy, or che-motherapy may be used along with surgery.
Immunotherapy may also be helpful. For patients with bilateral tumors or
can-cer of a functional single kidney, nephron-sparing surgery (par-tial
nephrectomy) may be considered. Favorable results have been achieved in
patients with small local tumors and a normal contra-lateral kidney.
Nephron-sparing surgery is increasingly being used to treat patients with solid renal lesions. The technical success rate of nephron-sparing
surgery is excellent, and operative morbidity and mortality are low. For renal
cell carcinoma, long-term cancer-free survival is comparable to that after
radical nephrectomy, par-ticularly for low-stage disease (Uzzo & Novick,
2001). Although laparoscopic nephroureterectomy is a lengthier surgical
proce-dure, it has the same efficacy and is better tolerated by patients than
open nephroureterectomy for upper tract transitional cell carcinoma. As more
experience is gained with this type of surgery, surgical time will be reduced
(Chen & Bagley, 2000; Jabbour, Desgrandchamps, Cazin et al., 2000; Shalhav,
Dunn, Portis et al., 2000).
Renal Artery Embolization. In patients
with metastatic renal car-cinoma, the renal artery may be occluded to impede
the blood supply to the tumor and thus kill the tumor cells. After
angio-graphic studies are completed, a catheter is advanced into the renal
artery, and embolizing materials (Gelfoam, autologous blood clot, steel coils)
are injected into the artery and carried with the arterial blood flow to
occlude the tumor vessels mechanically. This decreases the local blood supply,
making removal of the kid-ney (nephrectomy) easier. It also stimulates an
immune response because infarction of the renal cell carcinoma releases
tumor-associated antigens that enhance the patient’s response to meta-static
lesions. The procedure may also reduce the number of tumor cells entering the
venous circulation during surgical manipulation.
After
renal artery embolization and tumor infarction, a char-acteristic symptom
complex called postinfarction syndrome oc-curs, lasting 2 to 3 days. The
patient has pain localized to the flank and abdomen, elevated temperature, and
GI symptoms. Pain is treated with parenteral analgesic agents, and acetaminophen
is administered to control fever. Antiemetic medications, restric-tion of oral
intake, and intravenous fluids are used to treat the GI symptoms.
PHARMACOLOGIC THERAPY
Currently,
no pharmacologic agents are in widespread use for treating renal cell
carcinoma. Depending on the stage of the tumor, percutaneous partial or radical
nephrectomy may be fol-lowed by treatment with chemotherapeutic agents. The use
of bi-ologic response modifiers such as interleukin-2 (IL-2) and topical
instillation of bacillus Calmette-Guerin (BCG) in the renal pelvis continue to
be studied, with both treatments currently used in clinical practice (Hvarness,
Krarup & Eldrup, 2001; Nonomura, Ono, Nozawa et al., 2000; Okubo, Ichioka,
Matsuta et al., 2001).
Patients
may be treated with IL-2, a protein that regulates cell growth. This may be
used alone or in combination with lymphokine-activated killer cells, which are
WBCs that have been stimulated by IL-2 to increase their ability to kill cancer
cells. Inter-feron, another biologic response modifier, appears to have a
direct antiproliferative effect on renal tumors. The study of these biologic
agents and new biologic response modifiers is a priority because nearly half of
all patients with renal cell carcinoma die within 5 years of diagnosis (Pizza,
De Vinci, LoConte et al., 2001).
Nursing Management
The
patient with a renal tumor usually undergoes extensive diag-nostic and
therapeutic procedures, including surgery, radiation therapy, and medication
(or systemic) therapy. After surgery, the patient usually has catheters and
drains in place to maintain a patent urinary tract, to remove drainage, and to
permit accurate measurement of urine output. Because of the location of the
sur-gical incision, the position of the patient during surgery, and the nature
of the surgical procedure, pain and muscle soreness are common.
The
patient requires frequent analgesia during the postopera-tive period and
assistance with turning. Turning, coughing, use of incentive spirometry, and
deep breathing are encouraged to prevent atelectasis and other pulmonary
complications. The pa-tient and family require assistance and support to cope
with the diagnosis and uncertainties about the prognosis.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care. The patient
is taught to inspect andcare for the incision and perform other general
postoperative care. Additionally, the patient learns about activity and lifting
restric-tions, driving, and use of pain medications. Instructions are provided
about follow-up care and when to notify the physician about problems (fever,
breathing difficulty, wound drainage, blood in the urine, pain or swelling of
the legs).
The
patient is encouraged to eat a well-balanced diet and to drink adequate liquids
to avoid constipation and to maintain an adequate urine volume. Education and
emotional support are pro-vided related to the disease process, treatment plan,
and continu-ing care because many patients are concerned about the loss of the
other kidney, the possible need for dialysis, or the recurrence of cancer.
Continuing Care. Follow-up
care is essential to detect signs ofmetastases and to reassure the patient and
family about the pa-tient’s status and well-being. The patient who has had
surgery for renal carcinoma should have a yearly physical examination and chest
x-ray because late metastases are not uncommon. All sub-sequent symptoms should
be evaluated with possible metastases in mind.
If
follow-up chemotherapy is necessary, the patient and fam-ily are informed about
the entire treatment plan or chemother-apy protocol, what to expect with each
visit, and how to notify the physician. Periodic evaluation of remaining renal
function (creatinine clearance, serum BUN and creatinine levels) may also be carried
out periodically. A home care nurse may monitor the patient’s physical status
and psychological well-being and coor-dinate other services and resources
needed by the patient.
Related Topics