Chapter: Medical Surgical Nursing: Management of Patients With Urinary Disorders
Cancer of the Bladder
CANCER
OF THE BLADDER
Cancer
of the urinary bladder is more common in people aged 50 to 70 years. It affects
men more than women (3:1) and is more common in whites than in African
Americans. Bladder cancer is the fourth leading cause of cancer in American
men, accounting for more than 12,000 deaths in the U.S. annually (American
Cancer Society, 2002). Bladder cancer has a high worldwide in-cidence (Amling,
2001). Bladder tumors account for nearly 1 in 25 cancers diagnosed in the
United States. There are two forms of bladder cancer: superficial (which tends
to recur) and invasive. About 80% to 90% of all bladder cancers are
transitional cell (which means they arise from the transitional cells of the
blad-der); the remaining types of tumors are squamous cell and ade-nocarcinoma.
Research has demonstrated that many individuals with bladder cancer for which a
total cystectomy is required go on to develop upper urinary tract tumors
(Amling, 2001; Huguet-Perez, Palui, Millan-Rodriguez et al., 2001).
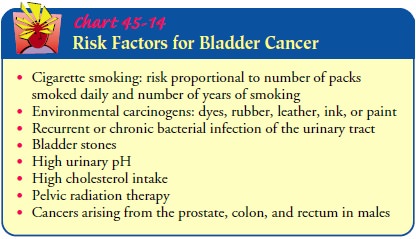
The
predominant cause of bladder cancer today is cigarette smoking. Cancers arising
from the prostate, colon, and rectum in males and from the lower gynecologic
tract in females may metas-tasize to the bladder (Chart 45-14).
Clinical Manifestations
Bladder
tumors usually arise at the base of the bladder and involve the ureteral
orifices and bladder neck. Visible, painless hematuria is the most common
symptom of bladder cancer. Infection of the urinary tract is a common
complication, producing frequency, urgency, and dysuria. Any alteration in
voiding or change in the urine, however, may indicate cancer of the bladder.
Pelvic or back pain may occur with metastasis.
Assessment and Diagnostic Findings
The
diagnostic evaluation includes cystoscopy (the mainstay of diagnosis),
excretory urography, a CT scan, ultrasonography, and bimanual examination with
the patient anesthetized. Biopsies of the tumor and adjacent mucosa are the
definitive diagnostic pro-cedures. Transitional cell carcinomas and carcinomas
in situ shed recognizable cancer cells. Cytologic examination of fresh urine
and saline bladder washings provide information about the prog-nosis,
especially for patients at high risk for recurrence of primary bladder tumors
(Amling, 2001).
Although
mainstay diagnostic tools such as cytology and CT scanning have a high
detection rate, they are costly. Newer diag-nostic indicators are being
studied. Bladder tumor antigens, nu-clear matrix proteins, adhesion molecules,
cytoskeletal proteins, and growth factors are being studied to support the
early detec-tion and diagnosis of bladder cancer. There are an increasing
number of molecular assays available for the detection of bladder cancer (Saad,
Hanbury, McNicholas et al., 2001).
Medical Management
Treatment
of bladder cancer depends on the grade of the tumor (the degree of cellular
differentiation), the stage of tumor growth (the degree of local invasion and
the presence or absence of metas-tasis), and the multicentricity (having many
centers) of the tumor. The patient’s age and physical, mental, and emotional
sta-tus are considered when determining treatment modalities.
SURGICAL MANAGEMENT
Transurethral resection or fulguration (cauterization) may be per-formed for simple papillomas (benign epithelial tumors). These procedures, eradicate the tumors through surgical incision or electrical current with the use of instruments inserted through the urethra. After this bladder-sparing surgery, intravesical administration of BCG is the treat-ment of choice.
Management
of superficial bladder cancers presents a challenge because there are usually
widespread abnormalities in the bladder mucosa. The entire lining of the
urinary tract, or urothelium, is at risk because carcinomatous changes can
occur in the mucosa of the bladder, renal pelvis, ureter, and urethra. About
25% to 40% of superficial tumors recur after transurethral resection or
fulgu-ration. Patients with benign papillomas should undergo cytology and
cystoscopy periodically for the rest of their lives because ag-gressive
malignancies may develop from these tumors.
A simple
cystectomy (removal of the bladder)
or a radical cystectomy is performed for invasive or multifocal bladder
can-cer. Radical cystectomy in men involves removal of the bladder, prostate,
and seminal vesicles and immediate adjacent perivesical tissues. In women,
radical cystectomy involves removal of the blad-der, lower ureter, uterus,
fallopian tubes, ovaries, anterior vagina, and urethra. It may include removal
of pelvic lymph nodes. Re-moval of the bladder requires a urinary diversion
procedure.
Although
radical cystectomy remains the standard of care for invasive bladder cancer in
the United States, researchers are ex-ploring trimodality therapy:
transurethral resection of the blad-der tumor, radiation, and chemotherapy.
This is in an effort to spare patients the need for cystectomy. A trimodality
approach to transitional cell bladder cancer mandates lifelong surveillance
with cystoscopy. Although most completely responding patients retain their
bladders free from invasive relapse, one quarter de-velop superficial disease.
This may be managed with transurethral resection of the bladder tumor and
intravesical therapies but carries an additional risk that late cystectomy will
be required (Zietman, Grocela & Zehr, 2001; Zietman, Shipley & Kaufman,
2000).
PHARMACOLOGIC THERAPY
Chemotherapy
with a combination of methotrexate, 5-fluorouracil, vinblastine, doxorubicin
(Adriamycin), and cisplatin has been ef-fective in producing partial remission
of transitional cell carci-noma of the bladder in some patients. Intravenous
chemotherapy may be accompanied by radiation therapy. The development of new
chemotherapeutic agents such as gemcitabine and the tax-anes has opened up
promising new perspectives in the treatment of bladder cancer. However, the
preliminary phase II data must be confirmed in adequately conducted phase III
trials (Bellmunt & Albiol, 2001).
Topical
chemotherapy (intravesical chemotherapy or instilla-tion of antineoplastic
agents into the bladder, resulting in contact of the agent with the bladder
wall) is considered when there is a high risk for recurrence, when cancer in
situ is present, or when tumor resection has been incomplete. Topical
chemotherapy de-livers a high concentration of medication (thiotepa,
doxorubicin, mitomycin, ethoglucid, and BCG) to the tumor to promote tumor
destruction. BCG is now considered the most effective in-travesical agent for
recurrent bladder cancer because it enhances the body’s immune response to
cancer.
Intravesical
BCG is an immunotherapeutic agent that is given intravesically and is effective
in the treatment of superficial tran-sitional cell carcinoma. BCG has a 43%
advantage in preventing tumor recurrence, a significantly better rate than the
16% to 21% advantage of intravesical chemotherapy. In addition, BCG is
par-ticularly effective in the treatment of carcinoma in situ, eradicat-ing it
in more than 80% of cases. In contrast to intravesical chemotherapy, BCG has
also been shown to decrease the risk of tumor progression.
The
optimal course of BCG appears to be a 6-week course of weekly instillations,
followed by a 3-week course at 3 months in tumors that do not respond. In
high-risk cancers, maintenance BCG administered for 3 weeks every 6 months may
limit recur-rence and prevent progression (Amling, 2001). The adverse ef-fects
associated with this prolonged therapy, however, may limit its widespread
applicability.
The
patient is allowed to eat and drink before the instillation procedure, but once
the bladder is full, the patient must retain the intravesical solution for 2
hours before voiding. At the end of the procedure, the patient is encouraged to
void and to drink lib-eral amounts of fluid to flush the medication from the
bladder.
RADIATION THERAPY
Radiation
of the tumor may be performed preoperatively to re-duce microextension of the
neoplasm and viability of tumor cells, thus reducing the chances that the
cancer may recur in the im-mediate area or spread through the circulatory or
lymphatic sys-tems. Radiation therapy is also used in combination with surgery
or to control the disease in patients with an inoperable tumor. The
transitional cell variety of bladder cancer responds poorly to chemotherapy.
Cisplatin, doxorubicin, and cyclophosphamide have been administered in various
doses and schedules and ap-pear most effective.
Bladder
cancer may also be treated by direct infusion of the cytotoxic agent through
the bladder’s arterial blood supply to achieve a higher concentration of the
chemotherapeutic agent with fewer systemic toxic effects. For more advanced
bladder can-cer or for patients with intractable hematuria (especially after
ra-diation therapy), a large, water-filled balloon placed in the bladder
produces tumor necrosis by reducing the blood supply of the bladder wall
(hydrostatic therapy). The instillation of formalin, phenol, or silver nitrate
relieves hematuria and strangury (slow and painful discharge of urine) in some
patients.
INVESTIGATIONAL THERAPY
The
use of photodynamic techniques in treating superficial blad-der cancer is under
investigation. This procedure involves systemic injection of a photosensitizing
material (hematoporphyrin), which the cancer cell picks up. A laser-generated
light then changes the hematoporphyrin in the cancer cell into a toxic
medication. This process is being investigated for patients in whom
intravesical chemotherapy or immunotherapy has failed (Amling, 2001).
Related Topics