Chapter: Medical Surgical Nursing: Management of Patients With Urinary Disorders
Lower Urinary Tract Infections
LOWER
URINARY TRACT INFECTIONS
Several
mechanisms maintain the sterility of the bladder: the physical barrier of the
urethra, urine flow, ureterovesical junction competence, various antibacterial
enzymes and antibodies, and antiadherent effects mediated by the mucosal cells
of the bladder. Abnormalities or dysfunctions of these mechanisms are
con-tributing factors to lower UTIs (Chart 45-2).
Pathophysiology
For
infection to occur, bacteria must gain access to the bladder, attach to and
colonize the epithelium of the urinary tract to avoid being washed out with
voiding, evade host defense mechanisms, and initiate inflammation. Most UTIs
result from fecal organ-isms that ascend from the perineum to the urethra and
the blad-der and then adhere to the mucosal surfaces.
BACTERIAL INVASION OF THE URINARY TRACT
By
increasing the normal slow shedding of bladder epithelial cells (resulting in
bacteria removal), the bladder can clear itself of even large numbers of
bacteria. Glycosaminoglycan (GAG), a hydro-philic protein, normally exerts a
nonadherent protective effect against various bacteria. The GAG molecule
attracts water mol-ecules, forming a water barrier that serves as a defensive
layer be-tween the bladder and the urine. GAG may be impaired by certain agents
(cyclamate, saccharin, aspartame, and tryptophan metabolites). The normal
bacterial flora of the vagina and ure-thral area also interfere with adherence
of Escherichia coli (the most common
microorganism causing UTI). Urinary immuno-globulin A (IgA) in the urethra may
also provide a barrier to bacteria.
REFLUX
An
obstruction to free-flowing urine is a problem known as ure-throvesical reflux, which is the reflux (backward flow) of
urinefrom the urethra into the bladder (Fig. 45-1). With coughing, sneezing, or
straining, the bladder pressure rises, which may force urine from the bladder
into the urethra. When the pressure returns to normal, the urine flows back
into the bladder, bringing into the bladder bacteria from the anterior portions
of the urethra. Ure-throvesical reflux is also caused by dysfunction of the
bladder neck or urethra. The urethrovesical angle and urethral closure pressure
may be altered with menopause, increasing the incidence of infec-tion in
postmenopausal women. Reflux is most often noted, how-ever, in young children.
Treatment is based on its severity.
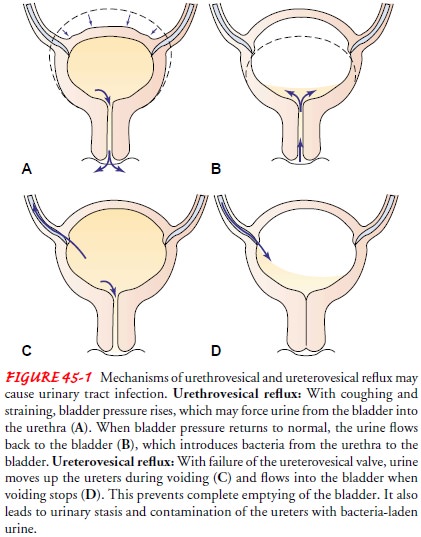
Ureterovesical or vesicoureteral reflux refers to the back-ward flow of urine from the bladder into one or both ureters (see Fig. 45-1). Normally, the ureterovesical junction prevents urine from traveling back into the ureter. The ureters tunnel into the bladder wall so that the bladder musculature compresses a small portion of the ureter during normal voiding. When the uretero-vesical valve is impaired by congenital causes or ureteral abnor-malities, the bacteria may reach and eventually destroy the kidneys.
UROPATHOGENIC BACTERIA
Bacteriuria is generally defined as more than 105colonies ofbacteria per
milliliter of urine. Because urine samples (especially in women) are commonly
contaminated by the bacteria nor-mally present in the urethral area, a
bacterial count exceeding 105 colonies/mL of clean-catch midstream urine is the
measure that distinguishes true bacteriuria from contamination. In men,
contamination of the collected urine sample occurs less fre-quently; hence,
bacteriuria can be defined as 104 colonies/mL urine. Community-acquired UTIs are
among the most common bacterial infections in women (Gupta, Hooton & Stamm,
2001).
The
organisms most frequently responsible for UTIs are those normally found in the
lower gastrointestinal (GI) tract. In a large-scale study of the types and
prevalence of organisms of patients with UTIs in both the community and
hospital setting, E. coli was
responsible for 54.7% of urinary tract infections. Isolation of E. coli is decreasing in comparison to
previous observations, especially in males and in patients with indwelling
bladder catheters, who instead had higher rates of Pseudomonas and En-terococcus
organisms than females and noncatheterized patients(Bonadio, Meini,
Spitaleri & Gigli, 2001).
ROUTES OF INFECTION
There
are three well-recognized routes by which bacteria enter the urinary tract: up
the urethra (ascending infection), through the bloodstream, (hematogenous
spread), or by means of a fistula from the intestine (direct extension).
The
most common route of infection is transurethral, in which bacteria (often from
fecal contamination) colonize the periurethral area and subsequently enter the
bladder by means of the urethra. In women, the short urethra offers little
resistance to the movement of uropathogenic bacteria. Sexual intercourse or
massage of the urethra forces the bacteria up into the bladder. This accounts
for the increased incidence of UTIs in sexually ac-tive women. Bacteria may
also enter the urinary tract by means of the blood (hematogenous spread) from a
distant site of infec-tion or through direct extension by way of a fistula from
the in-testinal tract.
Clinical Manifestations
A
variety of signs and symptoms are associated with UTI. About half of all
patients with bacteriuria have no symptoms. Signs and symptoms of uncomplicated
lower UTI (cystitis) include fre-quent pain and burning on urination,
frequency, urgency, noc-turia, incontinence, and suprapubic or pelvic pain. Hematuria
and back pain may also be present. In older individuals, these typ-ical
symptoms are seldom noted (see Gerontologic Considera-tions, below).
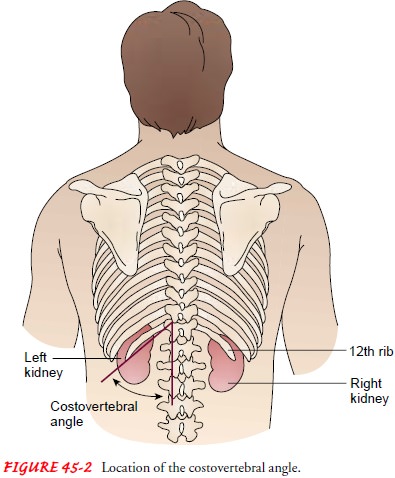
Signs
and symptoms of upper UTI (pyelonephritis) include fever, chills, flank or low
back pain, nausea and vomiting, head-ache, malaise, and painful urination.
Physical examination re-veals pain and tenderness in the area of the
costovertebral angles (CVA), which are the angles formed on each side of the
body by the bottom rib of the rib cage and the vertebral column (Fig. 45-2).
In patients with complicated UTIs, such as those with in-dwelling catheters, manifestations can range from asymptomatic bacteriuria to a gram-negative sepsis with shock. Complicated UTIs often are due to a broader spectrum of organisms, have a lower response rate to treatment, and tend to recur. Many pa-tients with catheter-associated UTIs are asymptomatic; however, any patient who suddenly develops signs and symptoms of septic shock should be evaluated for urosepsis.
Assessment and Diagnostic Findings
Results
of various tests, such as colony counts, cellular studies, and urine cultures,
help confirm the UTI diagnosis. The Ameri-can College of Obstetricians and
Gynecologists (ACOG) recom-mends that all pregnant women be screened for
asymptomatic bacteriuria since pregnancy itself is a risk factor for UTI
because the bladder does not empty as well as it normally does. In an
un-complicated UTI, the strain of bacteria will determine the anti-biotic of
choice.
COLONY COUNTS
UTI is
diagnosed by bacteria in the urine. A colony count of at least 105 colony-forming units
(CFU) per milliliter of urine on a clean-catch midstream or catheterized
specimen is a major crite-rion for infection. However, UTI and subsequent
sepsis have oc-curred with lower bacterial colony counts. About one third of
women with symptoms of acute infections have negative mid-stream urine culture
results and may go untreated if 105 CFU/mL is used as the criterion for
infection. The presence of any bacte-ria in specimens obtained by suprapubic
needle aspiration of the urinary bladder or catheterization is considered
indicative of infection.
CELLULAR STUDIES
Microscopic
hematuria (greater than 4 red blood cells [RBCs] per high-power field) is
present in about half of patients with acute infection. Pyuria (greater than 4 white blood cells [WBCs] per high-power
field) occurs in all patients with UTI; however, it is not specific for
bacterial infection. Pyuria can also be seen with kidney stones, interstitial
nephritis, and renal tuberculosis.
URINE CULTURES
Urine
cultures remain the gold standard in documenting a UTI and can identify the
specific organism present. Because of the high probability that the organism in
young women with their first UTI is E.
coli, cultures are often omitted. The following groups of patients should
have urine cultures obtained when bacteriuria is present:
· All men (because of the
likelihood of structural or func-tional abnormalities)
· All children
· Women with a history of
compromised immune function or renal problems
· Patients with diabetes
mellitus
· Patients who have
undergone recent instrumentation (in-cluding catheterization) of the urinary
tract
· Patients who were
hospitalized recently
· Patients with prolonged
or persistent symptoms
· Patients with three or
more UTIs in the past year
· Pregnant women
· Postmenopausal women
·
Women who are sexually active or have new partners
TESTING METHODS
Multistrip
dipstick testing for WBCs, known as the leukocyte es-terase test, and nitrite
testing (Griess nitrate reduction test) are common. If the leukocyte esterase
test is positive, it is assumed that the patient has pyuria (WBCs in the urine)
and should be treated. The Griess nitrate reduction test is considered positive
if bacteria that reduce normal urinary nitrates to nitrites are present.
Tests
for sexually transmitted diseases (STDs) may be per-formed because acute
urethritis caused by sexually transmitted or-ganisms (ie, Chlamydia trachomatis, Neisseria gonorrhoeae, herpes simplex) or
acute vaginitis infections (caused by Trichomonas
or Candida species) may be
responsible for symptoms similar tothose of UTI. Therefore, evaluation for STDs
may be performed.
Historically,
intravenous pyelography (IVP) was used to detect abnormalities in patients at
high risk for complicated or recurring UTI. Today, diagnostic studies such as
computed tomography (CT) and ultrasonography are preferred detection methods
for several reasons: CT scans may detect areas of pyelonephritis or ab-scesses,
and ultrasonography is extremely sensitive for detecting obstruction,
abscesses, tumors, and cysts. Transrectal ultrasonog-raphy (to assess the
prostate and bladder) is the procedure of choice for men with recurrent or
complicated UTIs. An IVP may be indicated to visualize the ureters or to detect
strictures or stones and is necessary for an accurate diagnosis of reflux
nephropathy. It is generally accepted that the first episode of UTI in women
does not require urologic evaluation (Hooton, Scholes, Stapleton et al., 2000).
Gerontologic Considerations
The
incidence of bacteriuria in the elderly differs from that in younger adults.
Bacteriuria increases with age and disability, and women are affected more
frequently than men. UTI is the most common cause of acute bacterial sepsis in
patients older than 65 years of age, in whom gram-negative sepsis carries a
mortality rate exceeding 50%. Urologists see many asymptomatic older pa-tients
with bacteriuria, and these individuals represent 20% of women over the age of
65. In the nursing home environment, up to 50% of females have asymptomatic
bacteriuria (Foxman, 2002).
In the
elderly population at large, structural abnormalities and neurogenic bladder
secondary to strokes or autonomic neuropa-thy of diabetes may prevent complete
emptying of the bladder and increase the risk for UTI. When indwelling
catheters are used, the risk for UTI rises dramatically as two or more
different strains of bacteria can be found in the urine of catheterized
pa-tients: in the urine itself, and on the surface of the catheter. El-derly
women often have incomplete emptying of the bladder and urinary stasis. In the
absence of estrogen, postmenopausal women are susceptible to colonization and
increased adherence of bacte-ria to the vagina and urethra. Oral or topical
estrogen has been used to restore the glycogen content of vaginal epithelial
cells and an acidic pH for some postmenopausal women with recurrent cystitis.
Local estrogen replacement may reduce the rate of UTIs in postmenopausal women
with recurrent UTIs (Raz, 2001).
The
antibacterial activity of prostatic secretions that protects men from bacterial
colonization of the urethra and bladder de-creases with aging. Although UTIs
are rare in men, the prevalence of infection in men older than 50 years of age
approaches that of women in the same age group. The dramatic rise in UTI in men
as they age is due largely to prostatic hyperplasia or carcinoma, strictures of
the urethra, and neuropathic bladder. The use of catheterization or cystoscopy
in evaluation or treatment may con-tribute further to the higher incidence of
UTI. The incidence of bacteriuria rises in men with confusion, dementia, or
bowel or bladder incontinence. The most common cause of recurrent UTI in the
elderly male patient is chronic bacterial prostatitis.
Transurethral
resection of the prostate gland may help to reduce its incidence.
In
institutionalized elderly patients, such as those in nursing homes, infecting
pathogens are often resistant to many antibi-otics. Factors that may contribute
to UTI in elderly nursing home patients include: high incidence of chronic
illness; frequent use of antimicrobial agents; infected pressure ulcers;
immobility and incomplete emptying of the bladder; and use of a bedpan rather
than a commode or toilet (Chart 45-3).
Diligent
hand hygiene, careful perineal care, and frequent toi-leting may decrease the
incidence of UTIs in nursing home pa-tients. The organisms responsible for UTIs
in the institutionalized elderly may differ from those found in patients
residing in the community; this is thought to be due in part to the frequent
use of antibiotic agents by patients in nursing homes. E. coli is the most common organism seen in elderly patients in the
commu-nity or hospital. Patients with indwelling catheters, however, are more
likely to be infected with Proteus,
Klebsiella, Pseudomonas, or Staphylococcus
species. Patients who have been previously treated with antibiotics may be
infected with Enterococcus species.
Fre-quent reinfections are common in older adults.
The
most common subjective presenting symptom of UTI in older adults is generalized
fatigue. The most common objective finding is a change in cognitive
functioning, especially in those with dementia, because these patients usually
exhibit even more profound cognitive changes with the onset of a UTI.
Medical Management
Management
of UTIs typically involves pharmacologic therapy and patient education. The
nurse is a key figure in teaching the patient about medication regimens and infection
prevention measures.
Controversy
continues about the need for treatment of asymp-tomatic bacteriuria in the
institutionalized elderly patient be-cause resulting antibiotic-resistant
organisms and sepsis may be greater threats to the patient. Most experts now
recommend with-holding antibiotics unless symptoms develop. Treatment
regi-mens, however, are generally the same as those for younger adults,
although age-related changes in the intestinal absorption of medications and
decreased renal function and hepatic flow may necessitate alterations in the
antimicrobial regimen. Renal function must be monitored and the dosage of
medications altered accordingly.
ACUTE PHARMACOLOGIC THERAPY
The
ideal treatment of UTI is an antibacterial agent that eradi-cates bacteria from
the urinary tract with minimal effects on fecal and vaginal flora, thereby
minimizing the incidence of vaginal yeast infections. (Yeast vaginitis occurs
in as many as 25% of pa-tients treated with antimicrobial agents that affect
vaginal flora. Yeast vaginitis often causes more symptoms and is more difficult
and costly to treat than the original UTI.) Additionally, the anti-bacterial
agent should be affordable and should produce few ad-verse effects and low
resistance. Because the organism in initial, uncomplicated UTIs in women is
most likely E. coli or other fecal
flora, the agent should be effective against these organisms. Various treatment
regimens have been successful in treating un-complicated lower UTIs in women:
single-dose administration, short-course (3 to 4 days) medication regimens, or
7- to 10-day therapeutic courses. The trend is toward a shortened course of
anti-biotic therapy for uncomplicated UTIs because about 80% of cases are cured
after 3 days of treatment.
In a
complicated UTI (ie, pyelonephritis), the general treatment of choice is
usually a cephalosporin or an ampicillin/amino-glycoside combination. Patients
in institutional settings may re-quire 7 to 10 days of medication for the
treatment to be effective. Other commonly used medications include
trimethoprim-sulfamethoxazole (TMP-SMZ, Bactrim, Septra) and nitrofurantoin
(Macrodantin, Furadantin). Occasionally, medications such as ampicillin or
amoxicillin are used, but E. coli
organisms have de-veloped resistance to these agents. Recent clinical trials
compar-ing the use of TMP-SMZ and the fluoroquinolone ciprofloxacin (Cipro)
found ciprofloxacin to be significantly more effective in community-based
patients and in nursing home residents (Gomolin & McCue, 2000; Talan et al.,
2000).
Levofloxacin
(Levaquin), another fluoroquinolone, is a good choice for short-course therapy
of uncomplicated, mild to mod-erate UTI. Clinical trial data show high patient
compliance with the 3-day regimen (95.6%) and a high eradication rate for all
pathogens (96.4%). Before using levofloxacin in patients with complicated UTIs,
the causative pathogen should be identified. Levofloxacin is used only when
generic and less costly antibiotics are likely to be ineffective (Bonapace et
al., 2000).
Nitrofurantoin
should not be used in patients with renal in-sufficiency because it is
ineffective at glomerular filtration rates (GFRs) of less than 50 mL/min and
may cause peripheral neurop-athy. Phenazopyridine (Pyridium), a urinary
analgesic, may be prescribed to relieve the discomfort associated with the
infection.
Regardless
of the regimen prescribed, the patient is instructed to take all the doses
prescribed, even if relief of symptoms occurs promptly. Longer medication
courses are indicated for men, preg-nant women, and women with pyelonephritis
and other types of complicated UTIs. In pregnant women, amoxicillin,
ampicillin, or an oral cephalosporin is used for 7 to 10 days.
LONG-TERM PHARMACOLOGIC THERAPY
Although
brief pharmacologic treatment of UTI for 3 days is usu-ally adequate in women,
infection recurs in about 20% of women treated for uncomplicated UTI.
Infections that recur within 2 weeks after therapy (referred to as a relapse)
do so because or-ganisms of the original offending strain remain in the vagina.
Re-lapses suggest that the source of bacteriuria may be the upper urinary tract
or that initial treatment was inadequate or adminis-tered for too short a time.
Recurrent infections in men are usu-ally due to persistence of the same
organism; further evaluation and treatment are indicated (Gupta et al., 2001;
Hooton et al., 2000; Stamm, 2001).
Reinfection
of the female patient with new bacteria is the rea-son for more than 90% of
recurrent UTIs in women. If the di-agnostic evaluation reveals no structural
abnormalities in the urinary tract, the woman with recurrent UTIs may be
instructed to begin treatment on her own whenever symptoms occur and to contact
the health care provider only when symptoms persist, fever occurs, or the
number of treatment episodes exceeds four in a 6-month period. This patient may
be taught to use dip-slide culture devices to detect bacteria.
If
infection recurs after completing antimicrobial therapy, another short course
(3 to 4 days) of full-dose antimicrobial therapy followed by a regular bedtime
dose of an antimicrobial agent may be prescribed. If there is no recurrence,
medication is taken every other night for 6 to 7 months. Other options in-clude
a dose of an antimicrobial agent after sexual intercourse, a dose at bedtime,
or a dose every other night or three times per week. Long-term use of
antimicrobial agents decreases the risk of reinfection and may be indicated in
patients with recurrent infections.
If
recurrence is caused by persistent bacteria from preceding infections, the
cause (ie, kidney stone, abscess), if known, must be treated. After treatment
and sterilization of the urine, low-dose preventive therapy (trimethoprim with
or without sulfamethox-azole) each night at bedtime is often prescribed.
Evidence
about the effectiveness of daily intake of cranberry extract or cranberry juice
to prevent UTIs in women is conflict-ing, although most randomized studies
point to a decrease in UTIs in women consuming daily cranberry juice
(Kontiokari, Sundqvist & Nuutinen, 2001).
Related Topics