Chapter: Psychology: Psychopathology
The Roots of Mood Disorders
The Roots of Mood Disorders
What
produces the mood disorders? Depression and bipolar disorder are thought to
result from multiple contributing factors, factors that include genetic,
neurochemical, and psychological influences.
GENETIC FACTORS
The
mood disorders have important genetic components. This is reflected in the fact
that the concordance rate is roughly two times higher in identical twins than
in frater-nal twins (Sullivan, Neale, & Kendler, 2000). The pattern is even
clearer for bipolar dis-order: If someone’s identical twin has the disorder,
there is a 60% chance that he, too, will have the disorder; the concordance
rate for fraternal twins is much lower, 12% (Kelsoe, 1997).
Adoption
studies point to the same conclusion, and the biological relatives of adopted
children with depression are themselves at high risk for depression (Wender,
Kety, Rosenthal, Schulsinger, & Ortmann, 1986). Likewise, the risk of
suicide is much higher among the biological relatives of depressed adoptees
than it is in the biological kin of nondepressed adoptees (Wallace, Schneider,
& McGuffin, 2002).
Importantly,
though, the genetic evidence indicates a clear distinction between depression
and bipolar disorder. The two disorders overlap in their symptoms (i.e.,
clinical depression resembles the depressed phase of bipolar disorder), but
they proba-bly arise from different sources. This is evident, for example, in
the fact that people with one of these disorders tend to have relatives with
the same condition but not the other. Apparently, then, there are separate
inheritance pathways for each, making it likely that they are largely separate
disorders (Gershon, Nurnberger, Berrettini, & Goldin 1985; Moffitt, Caspi,
& Rutter, 2006; Torgersen, 1986; Wender et al., 1986).
BRAIN BASES
Drugs
that influence the effects of various neurotransmitters can often relieve
symp-toms of mood disorders, and this suggests that these mood disorders arose
in the first place because of a disorder in neurotransmission. Three
neurotransmitters seem criti-cal for mood disorders: norepinephrine, dopamine,
and serotonin. Many of the anti-depressant and mood-stabilizing medications
work by altering the availability of these chemicals at the synapse (Miklowitz
& Johnson, 2006; Schildkraut, 1965).
How
these neurochemical abnormalities lead to mood disorders is uncertain, but it
is clear that these disorders involve more than a simple neurotransmitter
shortage or excess. In the case of depression, this is evident in the fact that
antidepressant drugs work almost immediately to increase the availability of
neurotransmitters, but their clinical effects usually do not appear until a few
weeks later. Thus, neurotransmitter problems are involved in depression (otherwise
the drugs would not work at all), but the exact nature of those problems
remains unclear.
In
the case of bipolar disorder, the mystery lies in the cycling between manic and
depressive episodes, especially since, in some patients, this cycling is quite
rapid and seemingly divorced from external circumstances. Some believe the
cycling is related to dysfunction in neuronal membranes, with the consequence
that the membranes mismanage fluctuations in the levels of various
neurotransmitters (Hirschfeld & Goodwin, 1988; Meltzer, 1986).
To
better understand the underlying brain bases of these mood disorders,
researchers have used both structural and functional brain imaging. Studies
using positron emission tomography (PET) show that severe depression is associated
with heightened brain acti-vation in a limbic system region known as the
subgenual cingulate cortex (Drevets, 1998). This finding makes sense, given
that inducing sadness in healthy participants leads to increased activation in
this brain region (Mayberg et al., 1999), as well as the evi-dence that when
depression is successfully treated, brain activity in this region returns to
normal levels (Mayberg et al., 1997).
In
the case of bipolar disorder, imaging studies suggest that adults with bipolar
dis-order have greater amygdala volumes than age-matched healthy controls
(Brambrilla et al., 2003). Functional-imaging studies parallel these structural
studies, showing greater brain activity in subcortical emotion-generative brain
regions such as the amyg-dala (Phillips, Ladouceur, & Drevets, 2008).
PSYCHOLOGICALRISKFACTORS
Our
account of the mood disorders also needs to take account of life experiences.
For example, depression and bipolar disorder are often precipitated by an
identifiable life crisis, whether that crisis involves marital or professional
difficulties, serious physical illness, or a death in the family (S. L.
Johnson, 2005a; Monroe & Hadjiyannakis, 2002; Neria et al., 2008). Broader
contextual factors, such as whether someone lives in a good or bad
neighborhood, may also influence whether a person develops depression, even
when controlling for risk factors associated with the person’s age, ethnicity,
income, education, and employment status (Cutrona, Wallace, & Wesner,
2006). The impor-tance of psychological factors is also evident in the fact
that individuals with mood dis-orders are at much greater risk for relapse if
they return after hospitalization to families who show high levels of criticism
and hostility (Hooley, Gruber, Scott, Hiller, & Yurgelin-Todd, 2005;
Miklowitz, 2007; Segal, Pearson, & Thase, 2003).
As
we mentioned earlier, though, personal and environmental stresses do not, by
themselves, cause mood disorders. What we need to ask is why some people are
unable to bounce back after a hard blow and why, instead of recovering, they
spiral downward into depression.
Part
of the explanation may be genetic, and some researchers are focusing on a gene
that regulates how much serotonin is available at the synapse. As discussed,
the gene itself is not the source of depression; instead, the gene seems to
create a vulner-ability to depression. The illness itself will emerge only if
the vulnerable person also experiences some significant life stress (Caspi et
al., 2003). However, this finding has been controversial, and research in this
area is ongoing (e.g., Munafo, Durrant, Lewis, & Flint, 2009; Risch et al.,
2009).
Another
part of the explanation for why stress puts some people at greater risk for
depression than others turns out to be social: severe stress is less likely to
lead to a mood disorder if a person has supportive family and friends (Brown
& Harris, 1978; Johnson et al., 1999; Joiner, 1997). Still another crucial
factor is how a person thinks about stressful events when they occur.
Many
depressed individuals—whether they are experiencing unipolar depression or are
in the depressive phase of bipolar disorder—believe that both they and the
world are hopeless and wretched. It seems plausible that these beliefs are
produced by the patient’s mood, but, according to the psychiatrist Aaron Beck,
the opposite is true, at least in the case of depression: The beliefs come
first; they produce the depression (see, for example, Beck, 1967, 1976). Beck
argues that depression stems from a set of intensely negative and irrational
beliefs: the beliefs some people hold that they are worthless, that their
future is bleak, and that whatever happens around them is sure to turn out for
the worst. These beliefs form the core of a negative cognitive schema by which a person interprets whatever
happens to her, leaving her mood nowhere to go but down.
A
related account of depression also focuses on how people think about what
happens to them. As we saw, people differ in how they explain bad events. Do we
think that a bad event happened because of something we did, so that, in some
direct way, we caused the event? Do we believe that similar bad events will
arise in other aspects of our lives? And do we think that bad events will
continue to happen to us, perhaps for the rest of our lives? Peterson and
Seligman propose that much depends on how we answer these questions, and,
moreover, they suggest that each of us has a consistent style for how we tend
to answer such questions—which they call an explanatory style. In their view, a person is vulnerable to
depression if her explanatorystyle tends to be internal (“I, and not some
external factor, caused the event”), global (“This sort of event will also
happen in other areas of my life”), and stable (“This is going to keep
happening”). This explanatory style is not by itself the source of depres-sion;
once again, we need to separate diathesis and stress. But if someone has this
explanatory style and then experiences a bad event, that person is at
considerably elevated risk for depression (Peterson & Seligman, 1984). In
addition, it appears that the explanatory style usually predates the
depression, with the clear implication that this way of interpreting the world
is not caused by depression but is instead a factor predisposing an individual
toward depression (Abramson et al., 2002; Alloy, Abramson, & Francis, 1999;
Peterson & Park, 2007).
SOCIAL AND CULTURAL RISK FACTORS
Clearly,
there are both biochemical and cognitive contributors to mood disorders. As we mentioned
earlier, though, mood disorders are also influenced by social settings. This is
evident, for example, in the fact that depression is less likely among people
with a strong social netowork of friends or family. The importance of social
surroundings is also visible in another way: the role of culture in shaping the
likelihood that depression will emerge, or the form that the disorder takes.
Depression
occurs in all cultures, and, in fact, the World Health Organization ranked
depression fourth among all causes of disability worldwide (Miller, 2006b).
However, its prevalence varies widely from one country to the next. For
example, depression is—not surprisingly— more common in countries such as
Afghanistan that
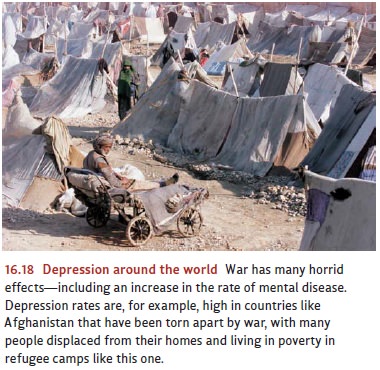
have
been torn apart by war (Bolton & Betancourt, 2004; Figure 16.18); the
difficulties in such countries also lead to other disorders, including
post-traumatic stress disorder. In contrast, depression is much less commonly
diagnosed in China, Taiwan, and Japan than in the West. When the disorder is
detected in these Asian countries, the symptoms are less often psychological
(such as sadness or apathy) and more often bodily (such as sleep dis-turbance,
weight loss, or, in China, heart pain; Kleinman, 1986; G. Miller, 2006a; Tsai
& Chentsova-Dutton, 2002). Why is this? There are several possibilities,
starting with the fact that cultures differ in their display rules for emotion , which will obvi-ously influence the
presentation and diagnosis of almost any mental disorder. In addition, people
in these Asian countries may differ in how they understand and perhaps even
expe-rience their own symptoms, and this, too, can influence diagnosis.
Even
within a single country, the risk of mood disorders varies. Depression, for
example, is more common among lower socioeconomic groups (Dohrenwend, 2000;
Monroe & Hadjiyannakis, 2002), perhaps because these groups are exposed to
more stress. In contrast, bipolar disorder is more common among higher socioeconomic groups (Goodwin
& Jamison, 1990), conceivably because the behaviors produced during a
person’s hypomanic phases may lead to increased accomplishment.
Related Topics