Chapter: Psychology: Psychopathology
Assessing Mental Disorders
Assessing Mental Disorders
In
addition to this general definition of mental disorder, the DSM gives definitions of the specific
mental disorders, definitions that we can use to decide which disorder—if any—a
person has. These “definitions” consist of lists of specific criteria, a certain
number of which must be met for a given disorder to be diagnosed. The diagnosis
is important because it is the first step both in understanding why a person is
suffering and (crucially!) in deciding how to help that person.
Mental
health professionals use the term assessment
to refer to the set of proce-dures for gathering information about an
individual, and an assessment may or may not lead to a diagnosis—a claim that
an individual has a specific mental disorder. Clinical assessment often
includes clinical interviews, self-report measures, and pro-jective tests. It
may also include laboratory tests such as neuroimaging or blood analyses that can inform the
practitioner about the patient’s physical well-being—for example, whether the
patient has suffered a stroke or taken a mood-alter-ing drug.
CLINICAL INTERVIEWS
Assessments
usually begin with a clinical interview, in which the clinician asks the
patient to describe her problems and concerns (Figure 16.5). Some aspects of
the inter-view will be open-ended and flexible, as the clinician explores the
patient’s current state and history. In addition, the clinician may rely on a semistructured interview, in which
specific questions are asked in a specific sequence, with attention to certain
types of content. For example, the clinician might use the Structured Clinical
Interview for DSM Disorders (SCID), which is designed to ask questions directly
pertinent to certain diagnostic categories.
Throughout,
the clinician will pay careful attention to the patient’s set of com-plaints,
or symptoms. Patients who say, “I
hear voices,” “I feel nervous all the time,” and “I feel hopeless” are
reporting symptoms. The clinician also looks for any objective signs that might accompany these
symptoms. If the same patients, respectively, turntoward a stapler as though it
were speaking, shake visibly, and look teary-eyed, these would be signs that
parallel the patients’ symptoms. Sometimes, though, symptoms do not correspond
to signs, and such discrepancies are also important. For example, a patient
might state, “My head hurts so bad it’s like there’s a buzz saw running through
my brain,” even thought the patient seems to be calm and unconcerned, and this
discrepancy, too, is informative.
The
full pattern of the patient’s symptoms and signs, taken together with their
onset and course, will usually allow the clinician to form an opinion as to the
specific disorder(s). This diagnosis is not set in stone, but serves as the
practitioner’s best judgment about the patient’s current state. The diagnosis
may well be revised as the clinician gains new information, including
information about how the patient responds to a particular form of treatment.
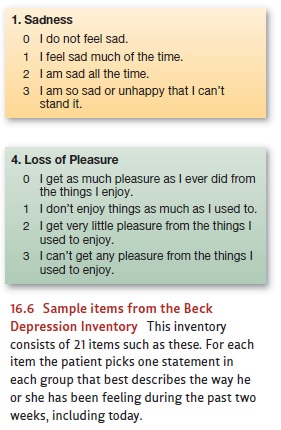
SELF –
REPORT MEASURES
In
some clinical assessments, a clinician will also seek information about a
patient by administering self-report measures. Some of these measures are
relatively brief and target a certain set of symptoms. These include measures
such as the Beck Depression Inventory (Beck, Steer, & Brown, 1996); sample
items from this inventory are shown in Figure 16.6. Other self-report measures
are much broader (and longer), such as the Minnesota Multiphasic Personality
Inventory, or MMPI. This test was developed in 1940 and was redesigned in 1989;
the current version, the MMPI-2, includes an imposing 567 items (Butcher,
Dahlstrom, Graham, Tellegen, & Kaemmer, 2001; Butcher et al., 1992).
To
construct the MMPI, its authors began with a large pool of test questions and
administered them to patients known to have a variety of different mental
disorders, as well as to a group of nonpatients. Next, they compared the
patients’ responses to those of the nonpatients. If all groups tended to
respond to a particular question in the same way, that question was deemed
uninformative and was removed from the test. A question was kept on the test
only if one of the patient groups tended to answer it differently from how the
nonpatient group answered it. The result was a test specifically
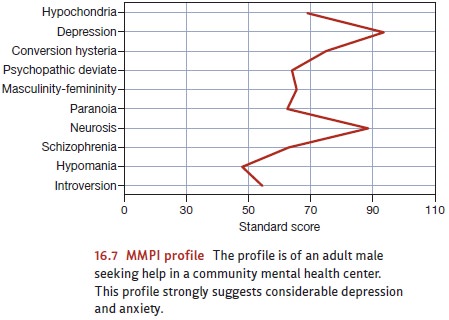
designed
to differentiate among patients with different mental disorders. Figure 16.7
shows an MMPI score profile.
PROJECTIVE TESTS
Some
clinicians supplement clinical interviews with what is called a projective
test. Advocates of projective tests argue that when the patient is asked to
respond to stimuli that are essentially unstructured or ambiguous, he cannot
help but impose a structure of his own, and, in the process of describing (or
relying on) this structure, he gives valuable information about unconscious
wishes and conflicts that could not be revealed by direct testing.
One
such test has the participant make up a story to describe what is going on in a
picture (the Thematic Apperception Test, or TAT; C. D. Morgan & Murray,
1935). Responses to these pictures are seen as revealing implicit or otherwise
hidden motives (Figure 16.8; McAdams, 1980; for variants on this procedure, see
McClelland, Koestner, & Weinberger, 1989; Winter, 1999). Another projective
test, the Rorschach Inkblot Test, has the patient describe what he sees in an
inkblot (Figure 16.9; Rorschach, 1921).
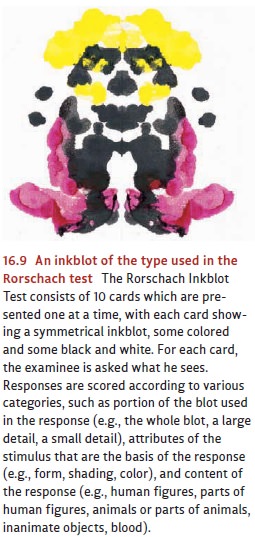
Projective
tests such as these are extremely popular—with more than 8 in 10 clini-cians
reporting that they use them at least occasionally (Watkins, Campbell,
Nieberding, & Hallmark, 1995). However, there is general agreement in the
research community that these tests’ popularity outstrips their demonstrated
validity. One review of Rorschach findings reported only small correlations
with mental health–related criteria (Garb, Florio, & Grove, 1998), and
there is ongoing debate about the role projective tests should play in diagnosis
(Garb, Wood, Nezworski, Grove, & Stejskal, 2001; Lilienfeld, Wood, &
Garb, 2000; Rosenthal, Hiller, Bornstein, Berry, & Brunell-Neuleib, 2001;
Westen & Weinberger, 2005).
Related Topics