Chapter: Psychology: Psychopathology
Conceptions of Mental Disorders
CONCEPTIONS OF
MENTAL
DISORDERS
We
have seen that people differ from one another in many ways, both in their
desirable qualities, like being intelligent or helpful, and in their
undesirable ones, like being selfish or aggressive. Even so, the attributes we
have considered all fall within the range that most people consider acceptable
or normal. In this, we consider differences that are outside the normal range
of variation— differences that carry us into the realm of mental disorders such
as depression, anxiety, and schizophrenia. These are conditions that cause
considerable suffer-ing and profoundly disrupt people’s lives—both the lives of
the people afflicted with the disorders and, often, the lives of others around
them.
The
study of mental disorders is the province of psychopathology, or, as it is sometimes called, abnormal
psychology. Like many corners of psychology, this domain has been studied
scientifically only in the last century. Concerns about mental illness,
however, have a much longer history. One of the earliest-known medical
documents, the Ebers papyrus (written about 1550 C.E.), refers to the disorder
we now know as depression (Okasha & Okasha, 2000). Other ancient cases
include King Saul of Judaea, who alternated between bouts of homicidal frenzy
and suicidal depression, and the Babylonian king Nebuchadnezzar, who walked on
all fours in the belief that he was a wolf (Figure 16.1). Across the millennia,
though, people have had very different concep-tions of what causes these
disorders.
Early Conceptions of Mental Disorders
The
earliest theories held that a person afflicted by a mental disorder was
possessed by evil spirits. As we will see, people tried various extreme
remedies to deal with this problem, such as flogging and starving, with the aim
of driving the evil spirits away.
In
recent centuries, a more sophisticated conception of mental disorders began to
develop—namely, that they are a type of disease, to be understood in the same
way as other illnesses. Proponents of this somatogenic
hypothesis (from the Greek soma,
meaning “body”) argued that mental disorders, like other forms of illness,could
be traced to an injury or infection. This position gained considerable
credibil-ity in the late nineteenth century, thanks to discoveries about general paresis.
General
paresis is a disorder characterized by a broad decline in physical and
psy-chological functions, culminating in marked personality aberrations that
may include grandiose delusions (“I am the king of England”) or profound
hypochondriacal depressions (“My heart has stopped beating”). Without
treatment, the deterioration progresses to the point of paralysis, and death
occurs within a few years. The break-through in understanding paresis came in
1897, when the Viennese physician Richard von Krafft-Ebing (1840–1902)
discovered that it was actually a consequence of infec-tion with syphilis. This
discovery paved the way for the development of antibiotics that could cure the
infection, and, if the drugs were given early enough, the symptoms of paresis
could be avoided altogether.
It
seems, then, that general paresis can be understood and treated like any other
medical problem. Should other forms of mental disorder be understood in the
same fashion—as the result of an infection or perhaps an injury? This view
gained many supporters in the late 1800s, including Emil Kraepelin (Figure
16.2), whose textbook, Lehrbuch der
Psychiatrie, emphasized the importance of brain pathology in
producingmental disorders.
However,
a somatogenic approach cannot explain all mental disorders. For example, more
than a hundred years ago, scholars realized that this approach was not
appropriate for the disorder then known as hysteria, which we encountered in
our discussion of psychoanalysis . Patients with hysteria typically showed odd
symptoms that seemed to be neurological, but with other indications that made
it plain there was no neurological damage. Some patients reported that their
limbs were paralyzed, but under hypnosis they could move their arms and legs
perfectly well, indicating that the nerves and muscles were fully functional.
Their symptoms, therefore, were not the result of a bodily injury; instead,
they had to be understood in terms of a psychogenic
hypothesis, which holds that the symptoms arise via psychological
processes.
Across
much of the late 19th and early 20th centuries, the most prominent version of
this hypothesis was Sigmund Freud’s, which described mental illness as
resulting from inner conflicts and defensive maneuvers aimed at dealing with
those conflicts. Early in the 20th century, other theorists offered alternative
conceptions of mental illness—but, like Freud, argued that the illness arose
from psychological processes, and not from bod-ily injury. For example, the
early behaviorists offered learning
models of mental illness, building on the mechanisms. In this view, many
mental disor-ders result from maladaptive learning and are best corrected with
remedial learning.
Modern Conceptions of Mental Disorders
Historically,
the somatogenic and psychogenic approaches were offered as sharply dis-tinct
proposals, and scholars debated the merits of one over the other. We now know
that both approaches have considerable validity. Biomedical factors play a
critical role in producing some forms of psychopathology; childhood experiences
and maladaptive learning contribute as well. As a consequence, each of these
approaches by itself is too narrow, and it would be a mistake to point to
either somatogenic or psychogenic factors as “the sole cause” of any disorder.
To understand why, let’s look more closely at the idea of cause in this domain.
DIATHESIS
- STRESS MODELS
Imagine
someone who goes through a difficult experience—perhaps the breakup of a
long-term relationship—and subsequently becomes depressed. We might be tempted
to say that the breakup caused the depression, but the breakup was not the only
force in play here. Many people experience breakups without becoming depressed;
this tells us that a breakup will cause depression only if other factors are
present.
What
are those other factors? Part of the answer lies in a person’s biology,
because, as we will see, some people have a genetic tendency toward depression.
This tendency remains unexpressed (and so the person suffers no depression)
until the person expe-riences a particularly stressful event. Then, when that
stressful event takes place, the combination of the event plus the biological
tendency will likely lead to depression.
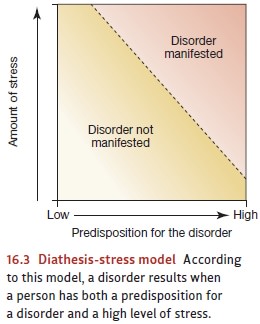
This
example suggests that we need a two-part theory of depression, and the same is
true for virtually every other form of psychopathology as well. This two-part
conception is referred to as a diathesis-stress
model (Bleuler, 1963; Meehl, 1962; Rosenthal, 1963), with one set of
factors (the diathesis) creating a
predisposition for the disorder, and a dif-ferent set of factors (the stress) providing the trigger that turns
the potential into the actual disorder (Figures 16.3). Notice that, by this
model, neither the diathesis nor the stress by itself causes the disorder;
instead, the disorder emerges only if both are present.
MULTICAUSAL MODELS
In
many cases, the diathesis takes the form of a genetic tendency—one that makes a
person vulnerable to depression if, during his lifetime, he encounters a
significant source of stress. It’s the combination of the vulnerability plus
the stress that leads to the illness. In other cases, the diathesis can take a
very different form. For example, a different factor may be how a person thinks about the events he
experiences—in particular, whether he tends to see himself as somehow
responsible for stressful, negative events . But, again, this style of
thinking, by itself, does not cause depression. Instead, the style of thinking
is only a diathesis: It creates a risk
or a vulnerability to depression, and if someone has this problematic thinking
style but leads a sheltered life—protected from the many losses and
difficulties faced by others—then he may never develop depression.
Examples
like these show the power of the diathesis-stress model, but they also reveal
that the model may be too simple. Often there are multiple diatheses for a particular indi-vidual and a particular
mental illness—including genetic factors, styles of thinking, and more.
Likewise, multiple factors often create the stress, including combinations of
harsh circumstances (for example, relationship difficulties or ongoing health
concerns) and spe-cific events (being the victim of a crime, perhaps, or
witnessing a devastating accident).
For
all these reasons, many investigators now adopt a multicausal model of depres-sion, which acknowledges that many
different factors contribute to the disorder’s emergence. Other mental
disorders also require a multicausal model. Indeed, to empha-size the diversity
of factors contributing to each disorder, most investigators now
urge
that we take a biopsychosocial
perspective, which considers biological factors (like genetics),
psychological factors (like a style of thinking), and social factors (like the
absence of social support; Figure 16.4).
Related Topics