Chapter: Psychology: Psychopathology
Defining Mental Disorders
Defining Mental Disorders
Phrases
such as “mental disorder” and “abnormal psychology” suggest that when defining
mental disorders, we should start with some conception of normalcy and then
define disorders as variations that are not normal. Thus, taking depression as
an example, we might acknowledge that everyone is occasionally sad, but we
might worry about (and try to treat) someone whose sadness is deeper and lasts
longer than normal sadness.
However,
this perspective invites difficulties, because even something normal can be
problematic. For example, almost everyone gets cavities, which makes them
normal, but this does not change the fact that cavities are a problem.
Likewise, many things are “abnormal” without necessarily being symptoms of
disorders. Pink is not a normal hair color, but this does not mean that someone
who dyes his hair pink is sick. It seems clear, therefore, that we cannot
equate being “abnormal” with being “ill.”
How,
then, should we define mental disorders? The most commonly accepted defi-nition
is the one provided by the American Psychiatric Association (2000) in the Diagnostic
and Statistical Manual of Mental Disorders (now in the text revisionof
its fourth edition, and hence known as the DSM-IV-TR; for the sake of
simplicity, we’ll refer to this work as DSM
from this point forward). The DSM
states that each of the mental disorders is a
Behavioral
or psychological syndrome or pattern that occurs in a person and that is
asso-ciated with present distress (e.g., a painful symptom) or disability
(i.e., impairment in one or more important areas of functioning) or with a
significantly increased risk of suffering death, pain, disability, or an
important loss of freedom. In addition, this syndrome or pattern must not be
merely an expectable and culturally sanctioned response to a particular event,
for example, the death of a loved one. Whatever its origi-nal cause, it must
currently be considered a manifestation of a behavioral, psychological, or
biological dysfunction in the individual.
Notice
that this is a functional definition—it focuses on distress and disability—
rather than one that specifies the causes or origins of the problem. Notice too
the requirement that the behaviors in question be not “expectable and
culturally sanc-tioned.” This aspect of the definition is important, because
what is expectable varies across cultures and over time, and so it’s valuable
to remind ourselves that we need to take social context into account when
assessing an individual’s thoughts, feelings, and behaviors.
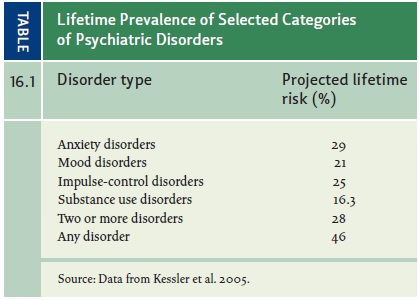
Using
this definition, we can tackle a crucial question: Just how common is mental
illness? Are we considering problems that are, in fact, relatively rare? Or is
mental illness common? Table 16.1 shows the prevalence of different psychiatric
disor-ders in the United States. The term prevalence
refers to how widespread a disorder is, and researchers typically consider two
types of prevalence. Point prevalence
refers to how many peo-ple in a given population have a given disorder at a
particular point in time. Lifetime
prevalence refers to how many people in a certain population will have the
disorder at any point in their lives. Reviewing this table, we can see that
nearly half of the U.S. population (46%) will experience at least one mental
disorder during their lifetimes, and more than a quarter (28%) will experience
two or more disorders. Most common are anxi-ety disorders (lifetime prevalence
rate of 29%) and impulse-control disorders (lifetime prevalence rate of 25%).
These statistics make it clear that large numbers of people suffer mental
disorders directly, and of course an even larger number of people (the friends,
family members, co-workers, and neighbors of the mentally ill) suffer
indirectly. We are, in short, talking
about a problem that is severe and widespread.
Related Topics