Chapter: Basic & Clinical Pharmacology : Antiseizure Drugs
Seizure Classification - Clinical Pharmacology of Antiseizure Drugs
CLINICAL
PHARMACOLOGY OF ANTISEIZURE DRUGS
SEIZURE CLASSIFICATION
In
general, the type of medication used for epilepsy depends on the empiric nature
of the seizure. For this reason, considerable effort has been expended to classify
seizures so that clinicians will be able to make a “seizure diagnosis” and on
that basis prescribe appropriate therapy. Errors in seizure diagnosis cause use
of the wrong drugs, and an unpleasant cycle ensues in which poor seizure
control is followed by increasing drug doses and medication toxic-ity. As
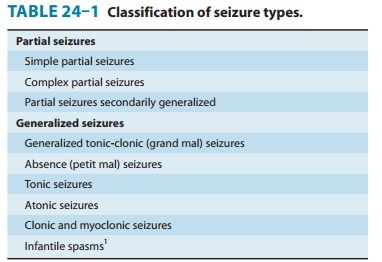
noted, seizures are divided into two groups: partial and generalized. Drugs
used for partial seizures are more or less the same for all subtypes of partial
seizures, but drugs used for general-ized seizures are determined by the
individual seizure subtype. A summary of the international classification of
epileptic seizures is presented in Table 24–1.
Partial Seizures
Partial
seizures are those in which a localized onset of the attack can be ascertained,
either by clinical observation or by electroen-cephalographic recording; the
attack begins in a specific locus in the brain. There are three types of
partial seizures, determined to some extent by the degree of brain involvement
by the abnormal discharge. The least complicated partial seizure is the simple partialseizure, characterized by
minimal spread of the abnormal dischargesuch that normal consciousness and
awareness are preserved. For example, the patient may have a sudden onset of
clonic jerking of an extremity lasting 60–90 seconds; residual weakness may
last for 15–30 minutes after the attack. The patient is completely aware of the
attack and can describe it in detail. The electroencephalogram may show an
abnormal discharge highly localized to the involved portion of the brain.
The
complex partial seizure also has a
localized onset, but the discharge becomes more widespread (usually bilateral)
and almost always involves the limbic system. Most complex partial seizures
arise from one of the temporal lobes, possibly because of the susceptibility of
this area of the brain to insults such as hypoxia or infection. Clinically, the
patient may have a brief warning followed by an alteration of consciousness
during which some patients stare and others stagger or even fall. Most,
however, demonstrate fragments of integrated motor behavior called automatisms for which the patient has
no memory. Typical automatisms are lip smacking, swallowing, fumbling,
scratching, and even walking about. After 30–120 seconds, the patient makes a
gradual recovery to normal consciousness but may feel tired or ill for several
hours after the attack.
The
last type of partial seizure is the secondarily
generalizedattack, in which a partial seizure immediately precedes a
general-ized tonic-clonic (grand mal) seizure. This seizure type is described
in the text that follows.
Generalized Seizures
Generalized
seizures are those in which there is no evidence of localized onset. The group
is quite heterogeneous.
Generalized tonic-clonic (grand mal) seizures are the
mostdramatic of all epileptic seizures and are characterized by tonic rigidity
of all extremities, followed in 15–30 seconds by a tremor that is actually an
interruption of the tonus by relaxation. As the relaxation phases become
longer, the attack enters the clonic phase, with massive jerking of the body.
The clonic jerking slows over 60–120 seconds, and the patient is usually left
in a stuporous state. The tongue or cheek may be bitten, and urinary inconti-nence
is common. Primary generalized tonic-clonic seizures begin without evidence of
localized onset, whereas secondary generalized tonic-clonic seizures are
preceded by another seizure type, usually a partial seizure. The medical
treatment of both primary and secondary generalized tonic-clonic seizures is
the same and uses drugs appropriate for partial
seizures.
The
absence (petit mal) seizure is
characterized by both sudden onset and abrupt cessation. Its duration is
usually less than 10 seconds and rarely more than 45 seconds. Consciousness is
altered; the attack may also be associated with mild clonic jerking of the
eyelids or extremities, with postural tone changes, auto-nomic phenomena, and
automatisms. The occurrence of automa-tisms can complicate the clinical
differentiation from complex partial seizures in some patients. Absence attacks
begin in child-hood or adolescence and may occur up to hundreds of times a day.
The electroencephalogram during the seizure shows a highlycharacteristic 2.5–3.5
Hz spike-and-wave pattern. Atypical absence patients have seizures with
postural changes that are more abrupt, and such patients are often mentally
retarded; the electroencepha-logram may show a slower spike-and-wave discharge,
and the sei-zures may be more refractory to therapy.
Myoclonic jerking is seen, to a greater or lesser extent, in
awide variety of seizures, including generalized tonic-clonic sei-zures,
partial seizures, absence seizures, and infantile spasms. Treatment of seizures
that include myoclonic jerking should be directed at the primary seizure type
rather than at the myoclonus. Some patients, however, have myoclonic jerking as
the major sei-zure type, and some have frequent myoclonic jerking and
occa-sional generalized tonic-clonic seizures without overt signs of neurologic
deficit. Many kinds of myoclonus exist, and much effort has gone into attempts
to classify this entity.
Atonic seizures are those in which the patient has sudden
lossof postural tone. If standing, the patient falls suddenly to the floor and
may be injured. If seated, the head and torso may suddenly drop forward.
Although most often seen in children, this seizure type is not unusual in
adults. Many patients with atonic seizures wear helmets to prevent head injury.
Momentary increased tone may be
observed in some patients, hence the use of the term “tonic-atonic seizure.”
Infantile spasms are an epileptic syndrome and not a
seizuretype. The attacks, though sometimes fragmentary, are most often
bilateral and are included for pragmatic purposes with the general-ized
seizures. These attacks are most often characterized clinically by brief,
recurrent myoclonic jerks of the body with sudden flex-ion or extension of the
body and limbs; the forms of infantile spasms are, however, quite
heterogeneous. Ninety percent of affected patients have their first attack
before the age of 1 year. Most patients are intellectually delayed, presumably
from the same cause as the spasms. The cause is unknown in many patients, but
such widely disparate disorders as infection, kernicterus, tuberous sclerosis,
and hypoglycemia have been implicated. In some cases, the electroencephalogram
is characteristic. Drugs used to treat infantile spasms are effective only in
some patients; there is little evidence that the cognitive retardation is
alleviated by therapy, even when the attacks disappear.
Related Topics