Chapter: Basic & Clinical Pharmacology : Antiseizure Drugs
Oxazolidinediones
OXAZOLIDINEDIONES
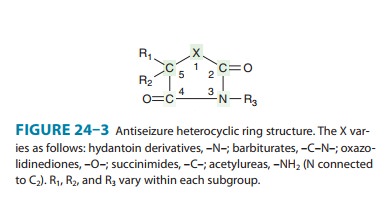
Trimethadione, the first oxazolidinedione (Figure 24–3),
wasintroduced as an antiseizure drug in 1945 and remained the drug of choice
for absence seizures until the introduction of succinim-ides in the 1950s. Use
of the oxazolidinediones—trimethadione, paramethadione, and dimethadione—is now
very limited; the lat-ter two are not readily available.These compounds are
active against pentylenetetrazol-induced seizures. Trimethadione raises the
threshold for seizure discharges after repetitive thalamic stimulation. It—or,
more notably, its active metabolite dimethadione—has the same effect on
thalamic Ca2+ currents as ethosuximide (reducing the T-type Ca2+
current). Thus, suppression of absence seizures is likely to depend on inhib-iting
the pacemaker action of thalamic neurons.Trimethadione is rapidly absorbed,
with peak levels reached within 1 hour after drug administration. It is not
bound to plasma proteins. Trimethadione is completely metabolized in the liver
by demethylation to dimethadione, which may exert the major antiseizure
activity. Dimethadione has an extremely long half-life (240 hours). The
therapeutic plasma level range for trimethadione has never been established,
although trimethadi-one blood levels higher than 20 mcg/mL and dimethadione
levels higher than 700 mcg/mL have been suggested. A dosage of 30 mg/kg/d of
trimethadione is necessary to achieve these levels in adults.The most common
and bothersome dose-related adverse effect of the oxazolidinediones is sedation.
Trimethadione has been asso-ciated with many other toxic adverse effects, some
of which are severe. These drugs should not be used during pregnancy.
Related Topics