Chapter: Basic & Clinical Pharmacology : Antihypertensive Agents
Drugs that Alter Sodium & Water Balance
DRUGS THAT ALTER SODIUM &
WATER BALANCE
Dietary
sodium restriction has been known for many years to decrease blood pressure in
hypertensive patients. With the advent of diuretics, sodium restriction was
thought to be less important. However, there is now general agreement that
dietary control of blood pressure is a relatively nontoxic therapeutic measure
and may even be preventive. Even modest dietary sodium restriction lowers blood
pressure (though to varying extents) in many hypertensive persons.
Mechanisms of Action & Hemodynamic
Effects of Diuretics
Diuretics
lower blood pressure primarily by depleting body sodium stores. Initially,
diuretics reduce blood pressure by reducing blood volume and cardiac output;
peripheral vascular resistance may increase. After 6–8 weeks, cardiac output
returns toward normal while peripheral vascular resistance declines. Sodium is
believed to contribute to vascular resistance by increasing vessel stiffness
and neural reactivity, possibly related to altered sodium-calcium exchange with
a resultant increase in intracellular calcium. These effects are reversed by diuretics
or sodium restriction.
Diuretics
are effective in lowering blood pressure by 10–15 mm Hg in most patients, and
diuretics alone often provide adequate treat-ment for mild or moderate
essential hypertension. In more severe hypertension, diuretics are used in
combination with sympathople-gic and vasodilator drugs to control the tendency
toward sodium retention caused by these agents. Vascular responsiveness—ie, the
ability to either constrict or dilate—is diminished by sympathople-gic and
vasodilator drugs, so that the vasculature behaves like an inflexible tube. As
a consequence, blood pressure becomes exqui-sitely sensitive to blood volume.
Thus, in severe hypertension, when multiple drugs are used, blood pressure may
be well controlledwhen blood volume is 95% of normal but much too high when
blood volume is 105% of normal.
Use of Diuretics
Thiazide
diuretics are appropriate for most patients with mild or moderate hypertension
and normal renal and cardiac function. More power-ful diuretics (eg, those
acting on the loop of Henle) such as furo-semide are necessary in severe hypertension,
when multiple drugs with sodium-retaining properties are used; in renal
insufficiency, when glomerular filtration rate is less than 30 or 40 mL/min;
and in cardiac failure or cirrhosis, in which sodium retention is
marked.Potassium-sparing diuretics are useful both to avoid excessive potassium
depletion and to enhance the natriuretic effects of other diuretics.
Aldosterone receptor antagonists in particular also have a favorable effect on
cardiac function in people with heart failure.Some pharmacokinetic
characteristics and the initial and usual maintenance dosages of
hydrochlorothiazide are listed in Table 11–2. Although thiazide diuretics are
more natriuretic at higher doses (up to 100–200 mg of hydrochlorothiazide),
when used as a single agent, lower doses (25–50 mg) exert as much
anti-hypertensive effect as do higher doses. In contrast to thiazides, the
blood pressure response to loop diuretics continues to increase at doses many
times greater than the usual therapeutic dose.
Toxicity of Diuretics
In
the treatment of hypertension, the most common adverse effect of diuretics
(except for potassium-sparing diuretics) is potassium depletion. Although mild
degrees of hypokalemia are tolerated well by many patients, hypokalemia may be
hazardous in persons taking digitalis, those who have chronic arrhythmias, or
those with acute myocardial infarction or left ventricular dysfunction.
Potassium loss is coupled to reabsorption of sodium, and restriction of dietary
sodium intake therefore minimizes potassium loss. Diuretics may also cause
magnesium depletion, impair glucose tolerance, and increase serum lipid
concentrations. Diuretics increase uric acid concentrations and may precipitate
gout. The use of low doses minimizes these adverse metabolic effects without
impairing the antihypertensive action. Potassium-sparing diuretics may
producehyperkalemia, particularly in patients with renal insufficiency and
those taking ACE inhibitors or angiotensin receptor blockers; spironolactone (a
steroid) is associated with gynecomastia.
Resistant Hypertension & Polypharmacy
Monotherapy of hypertension (treatment with a single drug) is desirable because compliance is likely to be better and cost is lower, and because in some cases adverse effects are fewer. However, most patients with hypertension require two or more drugs, preferably acting by different mechanisms (polyphar-macy). According to some estimates, up to 40% of patients may respond inadequately even to two agents and are considered to have “resistant hypertension.” Some of these patients have treat-able secondary hypertension that has been missed, but most do not and three or more drugs are required.
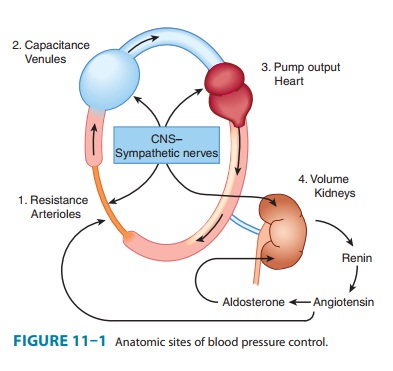
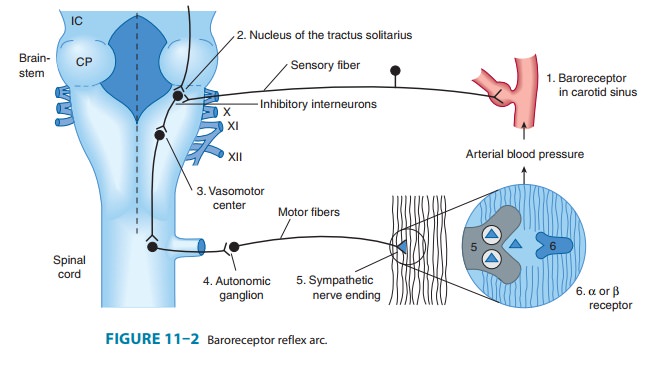
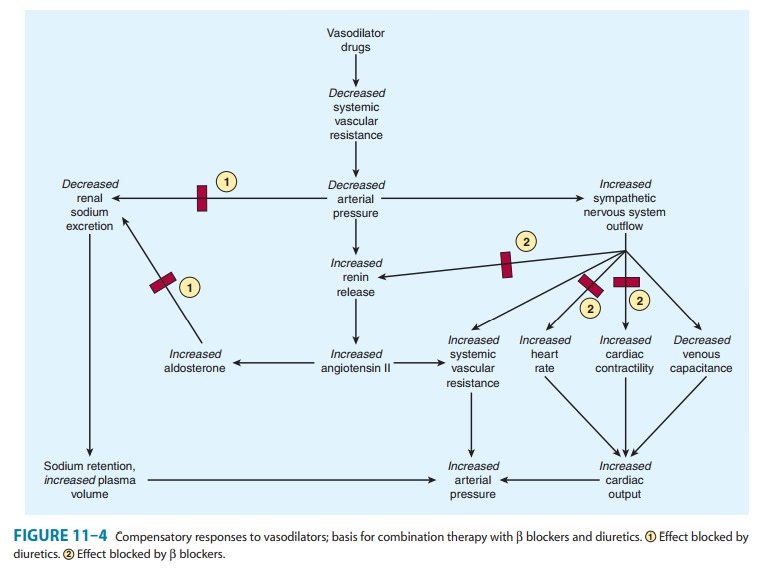
One rationale for polypharmacy in hypertension is that most drugs evoke compensatory regulatory mechanisms for maintain-ing blood pressure (see Figures 6–7 and 11–1), which may mark-edly limit their effect. For example, vasodilators such as hydralazine cause a significant decrease in peripheral vascular resistance, but evoke a strong compensatory tachycardia and salt and water retention (Figure 11–4) that is capable of almost completely reversing their effect. The addition of a β blocker prevents the tachycardia; addition of a diuretic (eg, hydrochloro-thiazide) prevents the salt and water retention. In effect, all three drugs increase the sensitivity of the cardiovascular system to each other’s actions.
A second reason is that some drugs have only modest maxi-mum efficacy but reduction of long-term morbidity mandatestheir use. Many studies of angiotensin-converting enzyme (ACE) inhibitors report a maximal lowering of blood pressure of less than 10 mm Hg. In patients with stage 2 hypertension (pressure 160/100 mm Hg), this is inadequate to prevent all the sequelae of hypertension, but ACE inhibitors have important long-term benefits in preventing or reducing renal disease in diabetic per-sons, and reduction of heart failure Finally, the toxicity of some effective drugs prevents their use at maximally effective dosage. The widespread indiscrimi-nate use of β blockers has been criticized because several large clinical trials indicate that some members of the group, eg, metoprolol and carvedilol, have a greater benefit than others, eg, atenolol. However, all β blockers appear to have similar ben-efits in reducing mortality after myocardial infarction, so these drugs are particularly indicated in patients with an infarct and hypertension.
In practice, when hypertension does not respond adequately to a regimen of one drug, a second drug from a different class with a different mechanism of action and different pattern of toxicity is added. If the response is still inadequate and compli-ance is known to be good, a third drug should be added. If three drugs (usually including a diuretic) are inadequate, dietary sodium restriction and an additional drug may be necessary
Related Topics