Chapter: Basic & Clinical Pharmacology : Antihypertensive Agents
Beta-Adrenoceptor-Blocking Agents
BETA-ADRENOCEPTOR–BLOCKING AGENTS
Of
the large number of β
blockers tested, most have been shown to be effective in lowering blood
pressure. The pharmacologic properties of several of these agents differ in
ways that may confer therapeutic benefits in certain clinical situations.
Propranolol
Propranolol
was the first β
blocker shown to be effective in hyper-tension and ischemic heart disease.
Propranolol has now been largely replaced by cardioselective β blockers such as
metoprolol and atenolol. All β-adrenoceptor–blocking agents are useful for
lowering blood pressure in mild to moderate hypertension. In severe
hypertension, β
blockers are especially useful in preventing the reflex tachycardia that often
results from treatment with direct vasodilators. Beta blockers have been shown
to reduce mortality after a myocardial infarction and some also reduce
mortality in patients with heart failure; they are particularly advantageous
for treating hypertension in patients with these conditions .
A. Mechanism and Sites of Action
Propranolol’s
efficacy in treating hypertension as well as most of its toxic effects result
from nonselective β
blockade. Propranolol decreases blood pressure primarily as a result of a
decrease in car-diac output. Other β blockers may decrease cardiac output or
decrease peripheral vascular resistance to various degrees, depend-ing on
cardioselectivity and partial agonist activities.
Propranolol
inhibits the stimulation of renin production by catecholamines (mediated by β1 receptors). It is
likely that propra-nolol’s effect is due in part to depression of the
renin-angiotensin-aldosterone system. Although most effective in patients with
high plasma renin activity, propranolol also reduces blood pressure in
hypertensive patients with normal or even low renin activity. Beta blockers
might also act on peripheral presynaptic β adrenoceptors to reduce sympathetic vasoconstrictor
nerve activity.
In
mild to moderate hypertension, propranolol produces a significant reduction in
blood pressure without prominent pos-tural hypotension.
B. Pharmacokinetics and Dosage
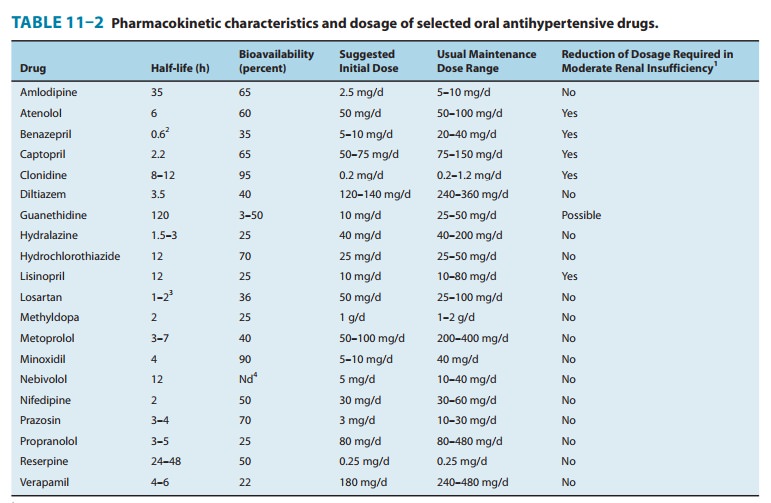
See
Table 11–2. Resting bradycardia and a reduction in the heart rate during
exercise are indicators of propranolol’s β-blocking effect, and changes in these
parameters may be used as guides for regulating dosage. Propranolol can be
administered twice daily, and slow-release preparations are available.
C. Toxicity
The
most important of these predict-able extensions of the β-blocking action occur in patients with
bradycardia or cardiac conduction disease, asthma, peripheral vascular
insufficiency, and diabetes.
When
propranolol is discontinued after prolonged regular use, some patients
experience a withdrawal syndrome, manifested by nervousness, tachycardia,
increased intensity of angina, and increase of blood pressure. Myocardial
infarction has been reported in a few patients. Although the incidence of these
com-plications is probably low, propranolol should not be discontinued
abruptly. The withdrawal syndrome may involve up-regulation or supersensitivity
of β
adrenoceptors.
Metoprolol & Atenolol
Metoprolol
and atenolol, which are cardioselective, are the most widely used β blockers in the
treatment of hypertension. Metoprolol is approximately equipotent to
propranolol in inhibit-ing stimulation of β1 adrenoceptors such as those in the heart but
50- to 100-fold less potent than propranolol in blocking β2 receptors. Relative
cardioselectivity may be advantageous in treating hyper-tensive patients who
also suffer from asthma, diabetes, or periph-eral vascular disease. Although
cardioselectivity is not complete, metoprolol causes less bronchial
constriction than propranolol at doses that produce equal inhibition of β1-adrenoceptor
responses. Metoprolol is extensively metabolized by CYP2D6 with high first-pass
metabolism. The drug has a relatively short half-life of 4–6 hours, but the
extended-release preparation can be dosed once daily (Table 11–2).
Sustained-release metoprolol is effective in reducing mortality from heart
failure and is particularly useful in patients with hypertension and heart
failure.
Atenolol
is not extensively metabolized and is excreted primarily in the urine with a
half-life of 6 hours; it is usually dosed once daily. Recent studies have found
atenolol less effective than metoprolol in preventing the complications of
hypertension. A possible reason for this difference is that once-daily dosing
does not maintain adequate blood levels of atenolol. The usual dosage is 50–100
mg/d. Patients with reduced renal function should receive lower doses.
Nadolol, Carteolol, Betaxolol, & Bisoprolol
Nadolol
and carteolol, nonselective β-receptor antagonists, are not appreciably
metabolized and are excreted to a considerable extent in the urine. Betaxolol
and bisoprolol are β1-selective blockers that are primarily metabolized in the liver
but have long half-lives. Because of these relatively long half-lives, these
drugs can be administered once daily. Nadolol is usually begun at a dosage of
40 mg/d, carteolol at 2.5 mg/d, betaxolol at 10 mg/d, and biso-prolol at 5
mg/d. Increases in dosage to obtain a satisfactory therapeutic effect should
take place no more often than every 4 or 5 days. Patients with reduced renal
function should receive corre-spondingly reduced doses of nadolol and
carteolol.
Pindolol, Acebutolol, & Penbutolol
Pindolol,
acebutolol, and penbutolol are partial agonists, ie, β blockers with some intrinsic sympathomimetic
activity. They lower blood pressure by decreasing vascular resistance and
appear to depress cardiac output or heart rate less than other β blockers, perhaps
because of significantly greater agonist than antagonist effects at β2 receptors. This may
be particularly beneficial for patients with bradyarrhythmias or peripheral
vascular disease. Daily doses of pindolol start at 10 mg; of acebutolol, at 400
mg; and of penbutolol, at 20 mg.
Labetalol, Carvedilol, & Nebivolol
These
drugs have both β-blocking
and vasodilating effects. Labetalol is formulated as a racemic mixture of four
isomers (it has two centers of asymmetry). Two of these isomers—the (S,S)-and (R,S)-isomers—are relatively inactive, a third (S,R)- is a potent α blocker, and the last (R,R)- is a potent β blocker. Labetalol has a 3:1 ratio of β:α antagonism after oral
dosing. Blood pressure is lowered by reduction of systemic vascular resis-tance
(via α
blockade) without significant alteration in heart rate or cardiac output.
Because of its combined α- and β-blocking activity, labetalol is useful in
treating the hypertension of pheo-chromocytoma and hypertensive emergencies.
Oral daily doses of labetalol range from 200 to 2400 mg/d. Labetalol is given
as repeated intravenous bolus injections of 20–80 mg to treat hyper-tensive
emergencies.
Carvedilol,
like labetalol, is administered as a racemic mixture. The S(–) isomer is a nonselective β-adrenoceptor blocker, but both S(–) and R(+)
isomers have approximately equalα-blockingpotency. The isomers are
stereoselectively metabolized in the liver, which means that their elimination
half-lives may differ. The aver-age half-life is 7–10 hours. The usual starting
dosage of carvedilol for ordinary hypertension is 6.25 mg twice daily.
Carvedilol reduces mortality in patients with heart failure and is therefore
particularly useful in patients with both heart failure and hypertension.
Nebivolol
is a β1-selective blocker with vasodilating properties that are not mediated by α blockade. D-Nebivolol has highly selec-tive β1 blocking effects,
while the L-isomer causes vasodilation; the drug is marketed as a racemic
mixture. The vasodilating effect may be due to an increase in endothelial
release of nitric oxide via induction of endothelial nitric oxide synthase. The
hemodynamic effects of nebivolol therefore differ from those of pure β blockers in that
peripheral vascular resistance is acutely lowered (by nebi-volol) as opposed to
increased acutely (by the older agents). Nebivolol is extensively metabolized
and has active metabolites. The half-life is 10–12 hours, but the drug can be
given once daily. Dosing is generally started at 5 mg/d, with dose escalation
as high as 40 mg, if necessary. The efficacy of nebivolol is similar to that of
other antihypertensive agents, but several studies report fewer adverse
effects.
Esmolol
Esmolol
is a β1-selective blocker that is rapidly metabolized via hydrolysis by
red blood cell esterases. It has a short half-life (9–10 minutes) and is
administered by constant intravenous infusion. Esmolol is generally
administered as a loading dose (0.5–1 mg/kg), followed by a constant infusion.
The infusion is typically started at 50–150 mcg/kg/min, and the dose increased
every 5 minutes, up to 300 mcg/kg/min, as needed to achieve the desired
therapeutic effect. Esmolol is used for management of intraoperative and postoperative
hypertension, and sometimes for hypertensive emergencies, particularly when
hypertension is asso-ciated with tachycardia.
Related Topics