Chapter: The Massage Connection ANATOMY AND PHYSIOLOGY : Cardiovascular System
Compensatory Adjustment - Regulation of the Cardiovascular System
COMPENSATORY ADJUSTMENT
The regulatory mechanism activity can be better ap-preciated by examining how they come into play during both everyday activities and abnormal condi-tions.
The compensatory adjustments made by the car-diovascular system to some of the challenges faced by the circulation, normally in everyday life and abnor-mally in disease, are considered below. The chal-lenges considered are:
Compensations for gravitational effects
1. Exercise
2. Shock
3. Cardiac Failure.
Compensations for Gravitational Effects
As a result of the effect of gravity when standing, the mean blood pressure in the feet of a normal adult is 180–200 mm Hg and the blood pressure in the head is about 60–75 mm Hg. If the person stands still, about 300–500 mL (31.7–53 qt) of blood tends to pool in the veins of the lower limbs and fluid tends to move out of the capillaries into the interstitial fluid as a result of the increased hydrostatic pressure (edema formation).
All this results in a reduction of blood returning to the heart and the stroke volume drops. If there were no compensatory mechanisms, the resultant drop in blood flow to the brain will result in prompt loss of consciousness.
The major compensation is caused by the stimula-tion of the carotid sinus and aortic arch baroreceptors when there is a slight drop in blood pressure. Stimu-lation results in immediate increase in heart rate to in-crease cardiac output and generalized vasoconstric-tion via the sympathetic nerves. In addition, there is an increase in renin levels, with formation of angiotensin II producing further vasoconstriction. Aldosterone lev-els also increase, conserving water, increasing blood volume, and maintaining blood pressure.
In the brain, local mechanisms play a part in in-creasing blood supply and maintaining conscious-ness. The accumulation of carbon dioxide, lack of oxygen, and changes in pH have a direct effect on blood vessels causing vasodilatation. Also, brain tis-sue extracts more oxygen from each unit of blood.
Prolonged standing, especially if standing still, produces additional problems because of the fluid moving into the interstitial compartment. As long as the person is moving, the contracting muscles com-press the veins and return blood to the heart. If the person stands still, venous return is decreased, and the person faints as a result of reduced brain perfu-sion. Fainting can be considered as a compensatory mechanism because, when the person falls to the ground, the effect of gravity is removed and venous return is restored.
Some people develop a fall in blood pressure, dizziness, dimness of vision, and even fainting when suddenly standing up. This is called orthostatic or postural hypotension. When the blood volume islow, as in dehydration, or when the compensatory mechanisms do not function well, as when taking an- tihypertensives or in those individuals with diabetes, the effects are more significant.
Effects of Acceleration
The effects of gravity on the circulation are multi-plied during acceleration or deceleration, whether on an elevator, a fast rides in an amusement park, or on a rocket. Gravity is measured by G force, with 1 G equal to the earth’s surface. The force is referred to as positive G when it is acting from head to foot, andnegative G when acting from foot to head. At acceler-ations equal to about 5 G, as a result of the excessive pooling of blood in the lower limbs and a drop in blood pressure and volume, vision fails in 5 seconds (blackout), and unconsciousness follows.
Negative G causes an increase in cardiac output and intense congestion of the head and neck vessels. A severe, throbbing headache and mental confusion (redout) result. Tiny blood vessels, especially around the eye, may rupture as a result of high blood pres-sure and congestion.
Exercise and Training
With exercise, extensive compensatory adjustments are made throughout the body, especially in the car-diovascular and respiratory systems.1
Muscle Blood Flow
At rest, muscle blood flow is as low as 2–4 mL/100 g (0.55–1.1 cu inches/lb) per minute. However, even the thought of exercise increases the blood flow via the sympathetic vasodilator fibers. When the muscle contracts, the blood vessels are compressed. If the tension reaches about 70% of maximum, no blood flows through the contracted muscles; however, when the muscle relaxes between contractions, blood flow increases significantly by autoregulation. The accu-mulation of local metabolites, increase in CO2 and decrease in O2 levels, etc., directly affect the smooth muscle of blood vessels to relax and more capillary beds to open. Fluid enters the interstitium faster and lymphatic flow is greatly increased. The increase in temperature and change in pH facilitates the absorp-tion of O2 from the hemoglobin and transport of CO2. All of these changes make it possible for the muscle to drastically speed its metabolism.
Changes in Systemic Circulation
The response of the systemic circulation to exercise depends on whether the exercise is isometric or iso-tonic (exercise is isometric when the muscle does notincrease in length when the tension increases, e.g., pushing against a wall).
In isometric exercise, the blood flow to the steadily contracting muscle is decreased as the vessels are compressed. The systolic and diastolic pressure in-creases significantly, and the heart has to work harder. In isotonic exercise, as a result of vasodilata-tion in the skeletal muscle, the blood pressure does not rise as much.
Cardiac output is increased by increasing both heart rate and stroke volume. The rise is in propor-tion to the severity of exercise. The cardiac output can sometimes exceed 35 L/minute. In children, the heart rate may be higher than 200 beats/minute dur-ing exercise. Venous return is significantly increased, aided by the contracting muscles and the suction ef-fect of rapid and deep inspiration. After stopping the exercise, the circulation returns to normal, and the recovery time depends on the severity of exercise and the fitness of the individual.
Temperature Regulation
Heat generated during exercise is dissipated by dila-tion of vessels to the skin. Some heat is lost in the ex-pired air as well. Increased production and evapora-tion of sweat are major sources of heat loss.
Effect of Training on the Cardiovascular System
Training produces changes in the heart and muscle that increases the efficiency of oxygen delivery.1The changes produced are related to the initial fitness level, genetic makeup, training frequency, training type, and training duration and intensity. Of the var-ious types of exercises some, such as aerobic exercise that exercises larger muscles, have greater effects on the cardiovascular system. Walking, running, cy-cling, and swimming are some examples of aerobic exercises.
Individuals who have had long-term aerobic train-ing have larger hearts, greater end-diastolic ventricu-lar volume, larger stroke volume and a lower heart rate, both at rest and during exercise. The larger heart enables them to increase cardiac output much more than individuals who are sedentary. Because of this increase in efficient use of energy, the heart is less taxed and does not have to increase the cardiac output as much as in sedentary individuals for the same intensity of exercise. The changes produced in the heart vary according to the type of exercise. For example, resistance-trained athletes (such as weight lifters) have a thicker ventricular wall compared with endurance athletes. But the endurance athletes tend to have a greater cavity size.
The resting heart rate of a trained athlete may be as low as 40–60 beats/minute. This is a result of the imbalance between sympathetic and parasympa-thetic stimulation of the heart caused by training.
At the microscopic level, training results in thick-ening of individual myofibrils and an increase in the number of myofilaments, mitochondria, enzymes, and blood flow per unit area of muscle. The changes produced are reversible and, if training is discontin-ued, decrease to pretraining levels within weeks.
With aerobic training, the plasma volume increases. This is a result of increased synthesis and production of albumin. The red blood cell mass is also increased with resultant increase in total blood volume.
With endurance training, more mitochondria and enzymes required for metabolism are present in the muscle. The number of capillaries per unit area is higher. The blood flow to the skeletal muscle in ques-tion is also increased. The result is better perfusion, with more availability of oxygen and less accumula-tion of metabolites.
Other changes that occur with regular exercise in-clude a reduction in blood pressure (both systolic and diastolic) and increased ability of the body to dissolve blood clots by facilitating fibrinolytic activity. In ad-dition, regular exercise reduces the incidence of anx-iety and depression and increases the overall sense of well-being. The incidence of numerous diseases is re-duced in those who exercise regularly.
Shock
Shock is a loosely-used term, with a great deal of con-fusion and controversy. There is a marked difference between the effects produced by electric shock, spinal shock, or shock in the circulatory system.
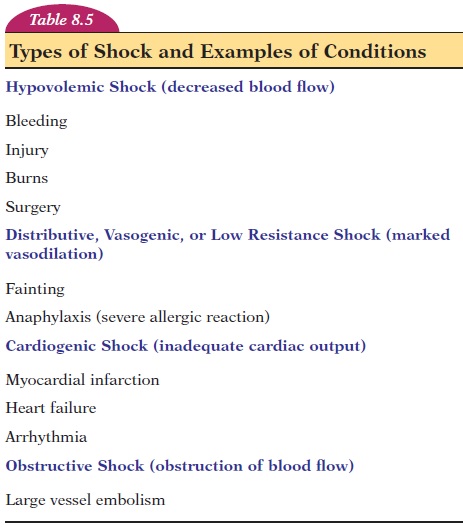
Shock in the circulatory system refers to conditions that cause profound and widespread reduction in the delivery of oxygen and nutrients to tissue.2There are many conditions that result in shock, a result of decreased blood volume; excessive dilation of blood ves-sels, with less blood reaching the heart and lungs; mal-functioning of the heart, or obstruction of blood flow in the lungs or heart. Table 8.5 lists the types of circu-latory shock, with examples of conditions.
The compensatory mechanisms in hemorrhagic and anaphylactic shock are discussed. The reduction in blood volume by bleeding reduces the venous re-turn and cardiac output, with a resultant drop in blood pressure. This drop is detected by the barore-ceptors, and there is a reflex increase in heart rate. There is profound vasoconstriction throughout the body (except in vessels of the brain and heart), and the skin appears pale and feels cool. Contraction of veins and the spleen try to increase the blood volume in the systemic circulation. The increase in breathing helps “suck” blood back to the heart. The increased secretion of vasopressin, renin, aldosterone, adrena-line, and noradrenaline try to bring the blood pres-sure and volume to normal levels. The thirst center is stimulated and urine production is decreased to in-crease blood volume by altering water intake and output.
If the vasoconstriction is prolonged, as in severe bleeding, there may be irreversible damage to the kidneys. After moderate bleeding, the plasma volume is restored within 12 to 72 hours by influx of tissue fluid. Erythropoietin levels increase, and the red cells return to normal in 4 to 8 weeks.
If bleeding is severe, the person cannot recover de-spite the presence of compensatory mechanisms and is said to be in irreversible shock. This is when the blood flow to the brain is so reduced that the cardiac and vasomotor centers stop functioning. Injury to the heart slows and eventually stops the heart.
In anaphylactic shock, which may occur when a person with allergies is reexposed to an allergen, the antigen-antibody reaction releases large quantities of histamine, causing dilation of arterioles and in-creased permeability of capillaries. Fluid moves out of the circulation, reducing blood volume and pres-sure. The same compensatory mechanisms as found in hypovolemic shock result.
Cardiac Failure
Cardiac failure is a condition in which the heart is unable to meet the demands made by the body. It in-variably happens when the heart is too weak to ade-quately pump the blood into the circulation. Because edema is one of the manifestations, a relatively com-mon sign observed in various disorders, cardiac fail-ure is considered. Depending on how severe and how fast the failure develops, a person may die, go into shock, or present with congestive cardiac failure.
To understand the signs and symptoms of conges-tive heart failure. Con-sider the pulmonary and systemic circulation as roads and imagine a partial roadblock in either the left or the right ventricle. Depending on traffic, the congestion and lineup of vehicles can be as far down as the leg. In cardiac failure, the blood returning to the heart is not pumped out adequately, and the pres-sure builds up in the vessels leading to the heart.
Now, if the left ventricle is failing, pressure builds up in the left atrium, pulmonary veins, capillaries, and pulmonary arteries; in short, the pulmonary cir-culation. As a result of the increased hydrostatic pres-sure, fluid moves out of the pulmonary capillaries into the alveoli of the lung with resultant pulmonaryedema. In this condition, the person has difficultybreathing (dyspnea).
Individuals with pulmonary edema feel better when sitting because the fluid tends to accumulate in the lower part of the lung due to gravity.
If the right ventricle fails, blood tends to backlog in the right atrium, vena cava, and circulation in vari-ous organs. The increased pressure in the right atrium is reflected by the jugular veins because no valve separates the vein from the atrium, and bulging neck veins can be observed. There is backlog in the liver, and it enlarges and presents as pain in the right upper abdomen, deep to the ribs. The buildup of pressure in the veins of the extremities (especially the legs) causes edema, which appears in the most de-pendent parts. In a supine position, the edema may be observed in the sacral region. If severe, fluid accu- mulates around the eye, and the face looks puffy. To-ward the end of the day, if the person has been up-right, the edema may be more in the dorsum of the foot and in the legs.
Because the heart does not pump adequately and tissue perfusion is reduced, the drop in pressure in the aortic arch and carotid artery is detected by the baroreceptors and the sympathetic nervous system is reflexively stimulated. All the regulatory mechanisms discussed come into play. Vasoconstriction and re-tention of water and sodium as a result of hormonal secretion occurs, worsening matters.
Heart failure treatment is directed at improving contractility of the heart, treating the symptoms, and reducing the load on the heart by eliminating the re-tained water with diuretics.
Related Topics