Chapter: Case Study in Obstetrics and Gynaecology: Peripartum Care and Obstetric Emergencies
Case Study Reports: Postpartum Bleeding
POSTPARTUM BLEEDING
History
A
39-year-old woman in her first
pregnancy delivered twin
sons 2 h ago. There
were no significant antenatal complications. She had been prescribed ferrous sulphate and folic
acid during the pregnancy as anaemia prophylaxis, and her last haemoglobin was 10.9
g/dL at 38 weeks.
The
fetuses were within
normal range for growth and liquor volume
on serial scan esti-
mations. A vaginal delivery was planned and she went into spontaneous labour at 38 weeks
and 4 days. Due to decelerations in the cardiotocograph (CTG) for the
first twin, both babies
were delivered by ventouse after
30 min active
pushing in the second stage. The midwife recorded both placentae as appearing complete.
As
this was a twin pregnancy, an intravenous cannula
had been inserted when labour was established and an epidural had been sited.
The lochia has
been heavy since
delivery but the woman
is now bleeding very heavily
and passing large
clots of blood.
On
arrival in the room you find that the sheets
are soaked with blood and there is also
approximately 500 mL of blood
clot in a kidney dish on the bed.
Examination
The
woman is conscious but drowsy and pale. The temperature is 35.9°C, blood
pressure 120/70 mmHg and heart rate 112/min.
The peripheries feel cool. The uterus is palpable to the
umbilicus and feels soft. The abdomen is otherwise soft and non-tender. On vaginal inspection there
is a second-degree tear which
has been sutured
but you are unable to assess further due to the presence
of profuse bleeding.
The
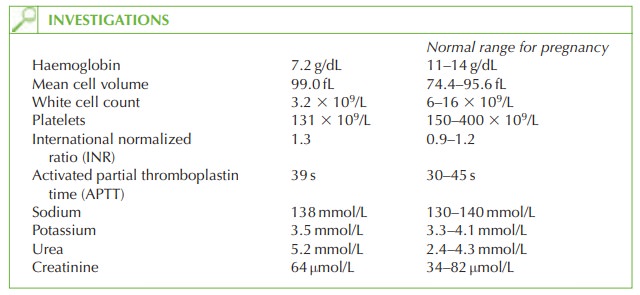
midwife sent blood
tests 30 min ago because
she was concerned about the blood
loss at the time.
Questions
·
What is the diagnosis
and what are the likely causes?
·
What is the sequence
of management options
you would employ
in this situation?
Answer:
The
diagnosis is primary
postpartum haemorrhage (PPH),
defined as the loss of more than 500
mL of blood in the first 24 h following
delivery. This classification applies even if the
blood is lost at Caesarean
section or while awaiting placental
delivery.
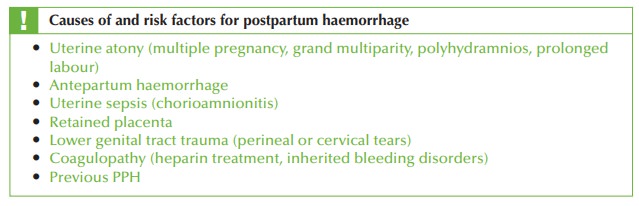
This woman’s major risk
factor is multiple pregnancy and with
the high uterus,
the cause is likely to be uterine atony (inability of the uterus to contract
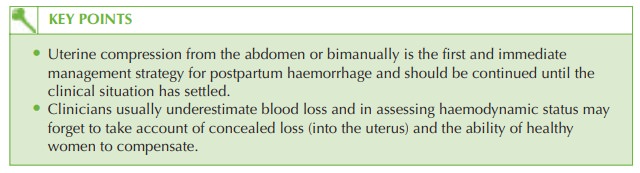
adequately). Blood loss is
often underestimated, the ‘high’ uterus
may contain a large volume
of concealed blood, and the blood pressure in young fit
women remains relatively normal until decompensa- tion occurs. Therefore this woman is in fact extremely sick and at risk of cardiac arrest
if immediate management is not employed.
The sequence of management
strategies is:
·
rub
up a contraction by placing
the dominant hand
over the uterus
and rubbing and squeezing firmly until the uterus becomes
firm
·
ensure two large-bore cannulae
are inserted with cross-matched blood
requested
·
recheck full blood count and coagulation
·
commence intravenous fluids for
volume expansion
·
give 500 μg ergometrine intramuscularly or intravenously to enhance
uterine contraction
·
start a syntocinon infusion
to maintain uterine
contraction
·
consider other uterotonics such as misoprostol or carboprost
·
transfer to theatre for
examination under anaesthetic to assess for
vaginal trauma, cer- vical laceration or retained
placental tissue
·
the
doctor or midwife
should continue bimanual
compression until the clinical situa- tion is under control
·
if
the bleeding does not settle
with the above
measures then further
options are uterine artery embolization or laparotomy with B-Lynch haemostatic suture, uterine artery
lig- ation or hysterectomy.
Related Topics