Chapter: Case Study in Obstetrics and Gynaecology: Peripartum Care and Obstetric Emergencies
Case Study Reports: Labour
LABOUR
History
A
midwife is concerned about a cardiotocograph (CTG) on the labour ward.
The woman is 42
years old and had an elective Caesarean section 3 years
ago for twins.
After counselling, she decided to opt for
a vaginal delivery in this pregnancy. She
is now 38 weeks 1 day’s
gestation and presented to the labour
ward an hour
ago. She was
found to have
contrac- tions, three in 10 min lasting
50 s each. There was no reported
rupture of membranes.
At
the time of arrival, examination revealed a symphysiofundal height of 39 cm, cephalic presentation and 3/5 palpable
abdominally. Vaginal
examination revealed intact mem-
branes with the head 1 cm above the ischial spines, occipitoanterior position
and the cervix 5 cm dilated.
She
was commenced on continuous CTG
monitoring (because of the previous Caesarean section), which showed
an initial baseline
rate of 135/min,
good variability, accelerations and no decelerations.
Twenty minutes ago spontaneous rupture of membranes occurred with clear liquor leaking.
Questions
·
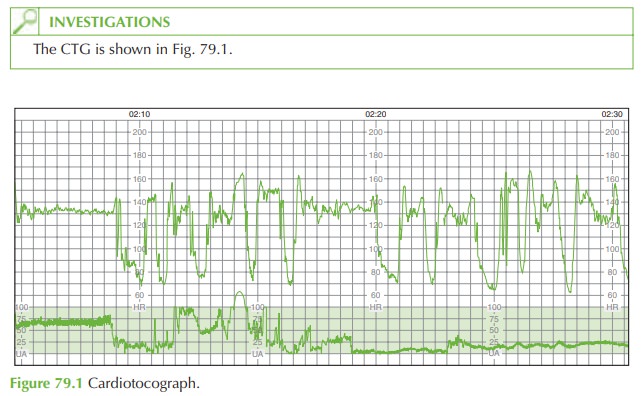
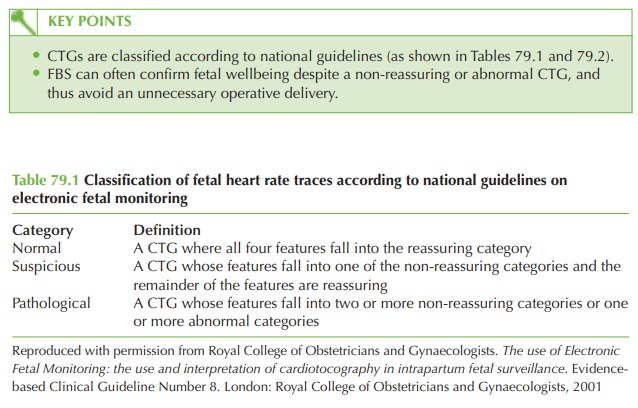
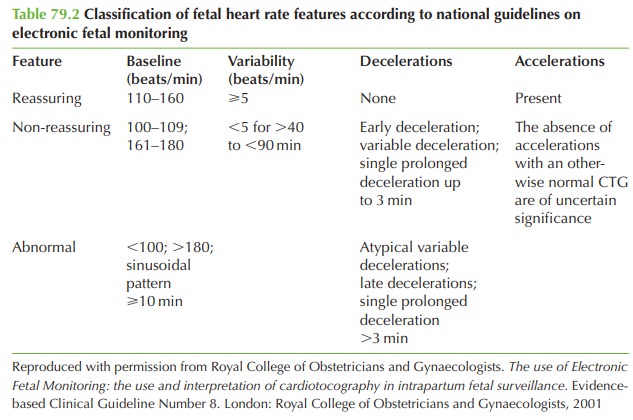
Describe and classify the CTG.
·
What are the possible
causes for this CTG pattern?
·
What should be your subsequent management?
Answer:
The
CTG shows a baseline rate of 130/min
and variability of 15/min. There
are variable decelerations to approximately 70/min
lasting 30–90 s. Although there
are no normal accelerations there is ‘shouldering’ before
and after the decelerations, a sign of the fetus increasing its heart rate in response
to the increased blood flow after the deceleration.
This CTG is unsatisfactory because
the tocometer is not registering contractions.
The
presence of variable decelerations with no other suspicious features leads to the clas- sification of this CTG as non-reassuring.
Management
In
this situation, the recent history
of spontaneous rupture
of membranes indicates imme- diate vaginal assessment to rule out
cord prolapse as the cause
of the suddenly abnormal CTG. This would
be a classic presentation for cord prolapse, though the condition itself is very rare.
Much more commonly variable
decelerations are caused by cord compression (by the uterine wall or, for
example, by the fetal hand)
If,
as is normally the case,
the cord is not palpable and the baby
is not easily
deliverable by instrumental delivery, then further assessment of fetal wellbeing is required as the abnor-
mality of the
CTG has already
lasted 20 min.
This should be by fetal
blood sampling (FBS).
In
this case FBS gave the following result: pH: 7.23
Base excess: —4.0 mmol/L
With a pH between
7.20 and 7.25,
it is reasonable to manage
the woman expectantly and repeat the FBS in 30 min. This was done and the second result
was:
pH: 7.22
Base excess: —5.1 mmol/L
At
this stage the woman was fully dilated
and pushing involuntarily, and the baby was
delivered spontaneously soon after the sample was taken.
In this case the fetal blood pH was relatively reassuring despite the dramatic appearance of the CTG. It is possible to avoid Caesarean section in such cases with appropriate use of FBS. It should be remembered that FBS is contraindicated in certain conditions such as maternal HIV, hepatitis or potential fetal-bleeding disorders.
Related Topics