Chapter: Case Study in Obstetrics and Gynaecology: Peripartum Care and Obstetric Emergencies
Case Study Reports: Pain in Pregnancy
PAIN IN PREGNANCY
History
A
28-year-old woman nulliparous woman is admitted
to the labour ward at 31 weeks and 6 days’ gestation, with abdominal pain.
In
this pregnancy she has had chronic low back pain for which
she has been under the physiotherapist. She
has also been
treated for confirmed urinary tract infections on two occasions. She underwent two large-loop excisions of the transformation zone (LLETZ)
procedures some years
ago. Since then her smears
have been normal,
the most recent being 10 months ago.
Yesterday she noticed an increase in her discharge with some dark vaginal bleeding
and abdominal discomfort. She thought the symptoms may have related
to something she had
eaten but she now feels
intermittent abdominal pain every few minutes, with no pain in
between episodes. Fetal movements are normal.
There is no history
of leaking of liquor. She has urinary
frequency, though this has not worsened recently. She is always constipated.
Examination
The
woman is apyrexial with blood pressure 109/60 mmHg and
heart rate 96/min. Symphysiofundal height is 30 cm and moderate contractions are
palpated lasting approxi- mately 35 s. The fetus
is breech on palpation and
the presenting part
feels engaged.
No
liquor is visible
on speculum examination. On vaginal examination the cervix is effaced and 3 cm dilated, with the breech
felt –2 cm above the ischial spines
and mem- branes intact.
Questions
·
What is the diagnosis?
·
What factors predispose to this?
·
How would you manage this woman?
Answer:
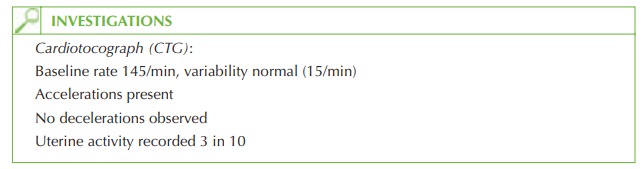
The
woman is in premature labour
– she has regular painful
contractions (as confirmed by the history, palpation and uterine activity
demonstrated on CTG) and the cervix is effaced
and dilated.
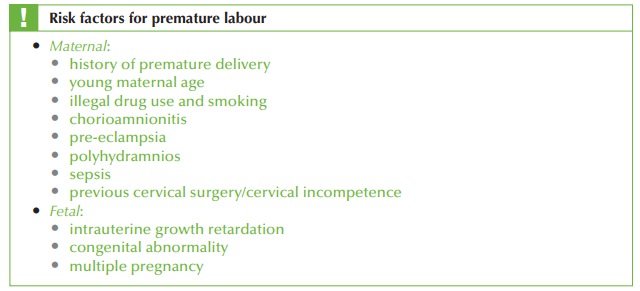
In
this history the possible risk factors are the LLETZ
procedures and urinary
tract infec- tions, raising
the possibility that she could be in premature labour due to a further untreated urinary tract infection. However, many women
in premature labour
have no obvious risk factors.
Management
·
Prevention of respiratory distress
syndrome (RDS):
·
antenatal corticosteroids (usually betamethasone intramuscular) prior to delivery
reduce the incidence of RDS
in premature infants, and ideally two
doses should be administered 12 h apart prior to delivery.
·
tocolysis (with atosiban, a beta-agonist or nifedipine) should
be started immedi- ately to try and
delay labour in order for
the steroids to be maximally effective (24 h), and then discontinued. The other indication for tocolysis is to settle
contrac- tions long enough
for in utero
transfer of the
mother to a unit with
facilities to care for a 31-week baby. In other situations tocolysis does not
seem to improve
fetal outcome, even though
it may prolong time to delivery.
·
Mode of delivery: although there
is evidence that
full-term singleton breech
babies should be delivered by Caesarean section
(rather than vaginally), there is no clear
evidence that this applies to preterm infants,
and as premature delivery is generally
reasonably quick, vaginal
delivery should be considered. The
contraindications to this would
be signs of fetal compromise on CTG, or maternal objection.
·
Postnatal care: the paediatric team should be informed of any woman
in actual or threatened preterm labour, in order
that appropriate arrangements are made for care
of the infant after delivery.
Related Topics