Chapter: Case Study in Obstetrics and Gynaecology: Peripartum Care and Obstetric Emergencies
Case Study Reports: Headache in Pregnancy
HEADACHE IN PREGNANCY
History
A
32-year-old woman who is 34 weeks’ gestation
has felt generally
unwell for 24 h. She has
a headache and
has noticed odd
visual symptoms such
as ‘wobbling’ of objects. She initially felt that she had a viral infection but the symptoms
are worsening and she thought she should get ‘checked
out’.
She
has epigastric discomfort and nausea. Her
legs have been
swollen for some
weeks but now her
hands and face
are puffy. The
baby has been
moving normally and
there is no lower abdominal pain and no bleeding
or abnormal discharge.
She
booked in the
pregnancy at 10 weeks
with a blood
pressure of 107/60 mmHg.
Booking blood tests and 12- and 20-week ultrasound scans were normal.
Examination
Her
blood pressure is 140/85 mmHg and pulse
rate 98/min. There
is moderate oedema
to the knees and she also appears digitally and facially oedematous. The fundi are normal.
On
abdominal palpation there is mild right upper quadrant and epigastric tenderness. The uterus is not tender and symphysiofundal height
measures 33 cm. The fetus
is cephalic and free,
with fetal parts
easily felt on palpation. Patellar reflexes are normal.
Questions
·
What is the likely diagnosis?
·
How
would you further
investigate and manage this patient?
ANSWER
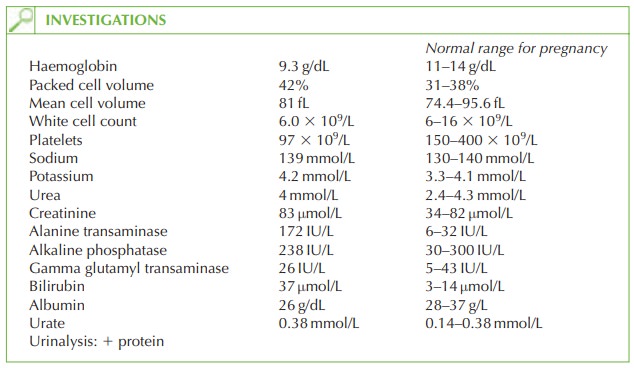
The
diagnosis is HELLP
syndrome (haemolysis, elevated
liver enzymes and low platelets).
HELLP syndrome is part
of the spectrum of pre-eclampsia, and
is a serious condition with a
relatively high maternal mortality (1 per
cent) and perinatal mortality (up to 60 per cent). Maternal complications include
placental abruption, renal
failure, liver failure
and disseminated intravascular coagulopathy (DIC). Fetal complications arise from prema- turity, abruption and
uteroplacental insufficiency.
The
diagnosis is made on the blood test results showing
the relevant features
of HELLP. In this case
there is also
pregnancy-induced hypertension and
proteinuria. However these clinical features do not
need to be present to make the
diagnosis of HELLP
syndrome.
HELLP may present antenatally or in
the first few days postpartum.
The
symptom of epigastric or right upper
quadrant pain should
always raise suspicion in a pregnant woman,
as it is a sign of liver
capsule stretching and may precede
liver rupture.
Investigation and management
The
woman needs urgent
delivery. This may be vaginal,
with regular monitoring of the blood test results and proteinuria every
6 h. Hourly blood pressure
should be recorded.
A
clotting screen is helpful to indicate any severe risk of bleeding
at delivery. If the cervix is unfavourable and the
woman is nulliparous then Caesarean section
may be considered, but the increased risk of associated bleeding should be borne in mind.
Fetal wellbeing should be checked
with cardiotocography and possibly ultrasound
for growth, liquor volume
and umbilical artery
Doppler. The fetal
parts being easily
palpable may be suggestive of oligohydramnios from
uteroplacental insufficiency.
Steroids should be administered to reduce the
chance of respiratory distress syndrome,
though there may be insufficient time before delivery for them to the effective.
Postnatally the woman should
be monitored in hospital for up to 5 days as the condition
may deteriorate before recovery. Once recovery occurs it is usually complete,
but there is an increased risk
of pre-eclampsia (and possibly HELLP syndrome) in subsequent pregnancies.
Related Topics