Chapter: Case Study in Obstetrics and Gynaecology: Peripartum Care and Obstetric Emergencies
Case Study Reports: Peripartum Collapse
PERIPARTUM COLLAPSE
History
A
woman aged 28 years is in labour
when she suddenly collapses. This is her fourth
preg- nancy and she
has had three
previous spontaneous vaginal
deliveries at term.
This preg- nancy has
been uncomplicated and
she has been
admitted with contractions at 37 weeks and 6 days.
On
arrival on the labour ward the fetus
was palpated to be normal
size, cephalic and 3/5
palpable abdominally. The cervix was 3 cm dilated and the membranes were intact. Blood pressure and urinalysis were normal. Initial
auscultation of the fetus was reassuring and the heart rate has continued to be
normal (around 140/min) on intermittent auscultation.
Five minutes ago spontaneous rupture
of membranes occurred during a contraction, with a large gush of clear fluid
from the vagina.
The woman reported an urge to push at that
stage and then became confused
and disorientated saying
that she could
not breathe and was
going to die. Immediately following this she collapsed.
Examination
The
woman is unconscious and unrouseable to painful stimuli.
The blood pressure
is 98/40 mmHg and heart rate 120/min. The oxygen saturation is 86 per cent on air and respiratory rate 20/min. The
heart sounds are
normal but on chest examination there are
inspiratory crackles throughout the chest.
The
abdomen is soft with intermittent contractions continuing, and in fact the fetal
head is now visible
at the perineum. There is no vaginal
bleeding.
Questions
·
What is the likely diagnosis and differential diagnosis?
·
How would you manage this woman?
Answer:
The
diagnosis is likely
to be an amniotic fluid
embolism. Differential diagnoses include:
·
pulmonary embolism
·
myocardial infarction
·
vasovagal attack.
The
factors leading to the diagnosis of amniotic fluid
embolism rather than one of the dif- ferentials are the history
of sudden collapse
without preceding chest
pain, and the fact
that this occurred around the time of rupture of membranes. Amniotic
fluid embolism is also often preceded
by premonitory symptoms, restlessness, confusion or cyanosis.
A vasovagal attack is very unlikely as this is usually associated with
bradycardia and would not account for the chest
signs or decreased oxygen saturation.
Amniotic fluid embolism occurs
when amniotic fluid
enters the maternal
circulation. This is usually
during labour but can occur
with maternal trauma
or very occasionally after delivery. It is rare (five
cases in the
last Confidential Enquiry
into Maternal and
Child Health 2000–2002), unpredictable, sudden and commonly fatal. Women
who die tend
to do so within an hour or so of becoming
unwell, having developed
acute hypoxia, coagu- lopathy and cardiac arrest.
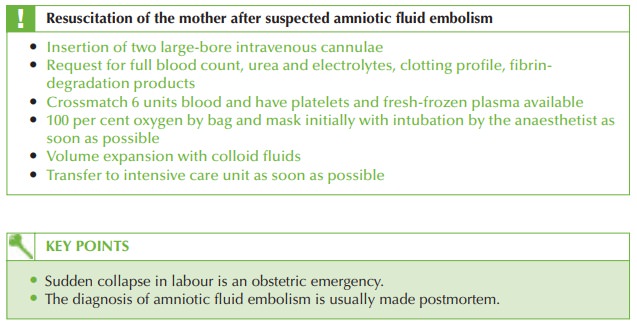
Management
The
baby should be delivered immediately as this will facilitate more effective resuscita- tion of the mother.
In this case a simple
forceps delivery should
be performed. If the baby was
not deliverable vaginally then immediate Caesarean section should be performed.
Massive postpartum haemorrhage is very likely
and syntocinon infusion
should be com- menced with further postpartum haemorrhage strategies such as ergometrine, carboprost, embolization or hysterectomy anticipated.
Related Topics