Chapter: Case Study in Obstetrics and Gynaecology: Peripartum Care and Obstetric Emergencies
Case Study Reports: Pain in Pregnancy
PAIN IN PREGNANCY
History
A
35-year-old woman arrives
on the labour ward complaining of abdominal pain and
vaginal bleeding at 36 weeks
2 days’ gestation. The pain started
2 h earlier while she
was in a café.
She describes constant
pain all over her abdomen
with exacerbations every
few minutes. It is not relieved by lying still
or by walking around. The
vaginal bleeding is bright red and was initially noticed
on the toilet paper and now has stained her under-
clothes and trousers. There are no urinary
or bowel symptoms.
The
baby has been moving
normally until today, but
the woman has not
paid any attention to the movements
since the pain started.
This is her first
pregnancy and until
now progress has
been uneventful with
shared care between the general practitioner and midwife. Both the 11–14-week and the anomaly
scan at 20 weeks
were reassuring. Booking
and subsequent blood
tests were normal.
The book- ing blood
pressure was 112/68 mmHg and the most recent
blood pressure 2 days ago was
128/80 mmHg.
Examination
She
is obviously in significant pain and feels clammy. She is apyrexial, her heart rate is
115/min and blood pressure
110/62 mmHg. The symphysiofundal height is 38 cm and the
uterus feels hard and is very tender.
It is not possible to feel the presentation of the fetus due to the uterine
tightening. On speculum
examination there is a trickle
of blood through the cervix and the cervix appears
closed. Vaginal
examination reveals that the cervix is
soft and almost full effaced
but closed. No fetal heart sounds are heard on auscultation
with the hand-held fetal Doppler. Ultrasound scan confirms that the fetus
has died.
Questions
·
What is the diagnosis?
·
How
do you interpret the examination and blood test findings?
·
How would you manage this patient?
Answer:
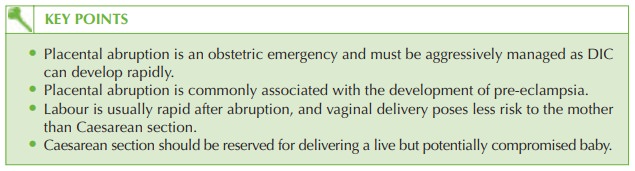
The pain and bleeding are due to placental abruption. In this case the presence
of vaginal blood classifies
it as a ‘revealed
abruption’ but the other signs of hardened
‘couvelaire’ uterus,
raised symphysiofundal height, tachycardia and low haemoglobin all suggest that the major part of the blood is still concealed.
This is an extremely important point as the amount
of visualized blood
can be misleading when there
may be 1–2 L of blood within
the uterus.
The
blood pressure appears
normal, but this is because
the woman is relatively young
and fit – she is able to compensate by increasing heart
rate and cardiac
output for some time.
By the time her blood pressure falls she has decompensated and is critically unwell, so normal blood
pressure in young
people should always
be interpreted carefully. If her blood pressure were checked lying
and standing, there
would be a significant difference, which would reveal the extent of her hypovolaemia.
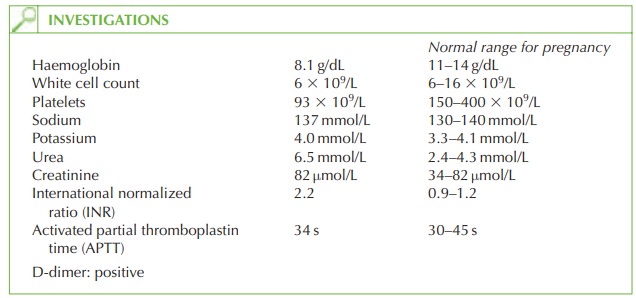
The
increase in INR, decreased platelets and positive D-dimer
test (a reflection of raised
fibrin-degradation products) confirm
that the woman
has developed disseminated intravascular coagulopathy (DIC) as a result of the abruption.
The
fetus has died
(intrauterine fetal death)
because the placenta has separated from
the uterus and the
uteroplacental circulation has
therefore been interrupted.
Management
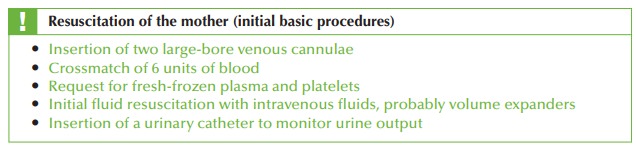
This is an obstetric emergency as the
woman is hypovolaemic and has developed a coag- ulopathy. The
management centres on correction of the clotting and volume replacement as well as delivery
of the baby. The anaesthetist and senior obstetrician should liaise
closely in management.
As
the baby has
died there is no indication for Caesarean section, which would put
her at risk of further bleeding. Therefore vaginal induction of labour should
be initiated. Labour is often rapid after
an abruption, and as the cervix is fully effaced
and soft it may be suf-
ficient to perform artificial rupture
of membranes (ARM)
to initiate the process of deliv-
ery. At ARM, a large amount
of blood is likely to be apparent.
A
syntocinon infusion should
be commenced immediately after delivery as uterine atony and postpartum haemorrhage are
common after significant abruption.
Related Topics