Chapter: Case Study in Obstetrics and Gynaecology: Peripartum Care and Obstetric Emergencies
Case Study Reports: Labour
LABOUR
History
A
22-year-old woman is admitted to the labour
ward for induction of labour at 39 weeks’ gestation. This is her first ongoing
pregnancy, having had a first-trimester miscarriage 13 months previously. She booked at 9 weeks
and had normal
booking blood tests, and 11–14-week scan and 21-week
anomaly scan did not show any obvious
fetal abnor- mality. Blood pressure and urinalysis have always been normal.
At her 32 week midwife appointment
she reported feeling very uncomfortable abdom-
inally, and the midwife measured
the symphysiofundal height
to be 36 cm. A further ultra- sound scan was therefore requested
whish showed normal fetal growth but increased
liquor volume. She had been reviewed in the antenatal
clinic and was tested for gesta-
tional diabetes with glucose tolerance test but this was normal. Subsequent
examinations had again confirmed an increased symphysiofundal height, and further
ultrasound scan at 36 weeks again showed normal growth,
no fetal abnormality and markedly increased liquor volume. The fetal
movements had always
been normal.
A
decision had been made for induction of labour at 40 weeks
because the woman
had become so uncomfortable and breathless.
On palpation the fetus was cephalic
with the head 4/5 palpable abdominally. Cardio-
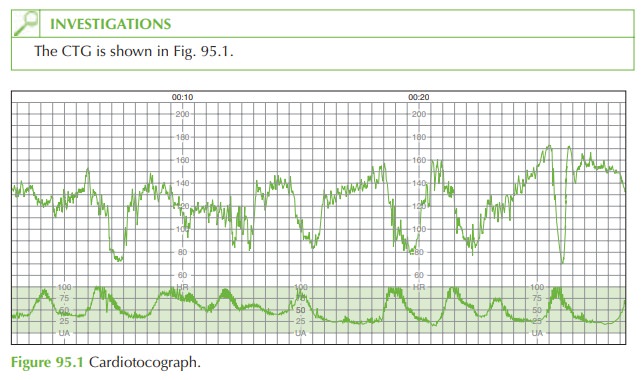
tocograph (CTG) was reassuring; 2 mg of prostaglandin gel had been inserted into the
posterior fornix of the vagina
and CTG monitoring continued for a further 20 min.
The
woman then mobilized and contractions started
within an hour.
She requested an epidural for analgesia and while this was being
prepared CTG monitoring was com- menced. At this stage,
spontaneous rupture of membranes occurred
with a very large vol- ume
of clear liquor soaking the bed sheets.
Questions
·
Describe the CTG
·
What is the likely diagnosis?
·
How
would you confirm
the diagnosis and manage this situation?
ANSWER
The
CTG shows deep variable decelerations. The sudden CTG deterioration after
rupture of membranes in a woman with polyhydramnios suggests the likelihood of prolapse of the
cord. Other possible diagnoses are placental abruption or fetal head compression from precipitate labour. The diagnosis is easily confirmed with vaginal examination. A loop of umbilical cord will be palpated in the vagina and will be pulsatile.
This is an obstetric emergency and the emergency bell should be activated with the
senior midwife, theatre
team, senior obstetrician, paediatrician and anaesthetist sum- moned immediately.
The important management steps are:
·
the
examiner should not
remove their fingers
from the vagina
and should attempt
to elevate the fetal head above the cord and minimize
contact with the cord to prevent
spasm
·
the
woman should be rotated into
the ‘all-fours position’ (head lower than
buttocks), which will facilitate relieving the weight
of the baby and abdomen
from the prolapsed cord
·
she
should be transferred to theatre immediately for Caesarean section
·
intravenous access should be
obtained, and a general anaesthetic administered, using a rapid sequence
induction with cricoid
pressure
·
the
examiner should only remove their
fingers from the presenting part in the vagina
when the uterus has been opened and the baby is being delivered.
Related Topics