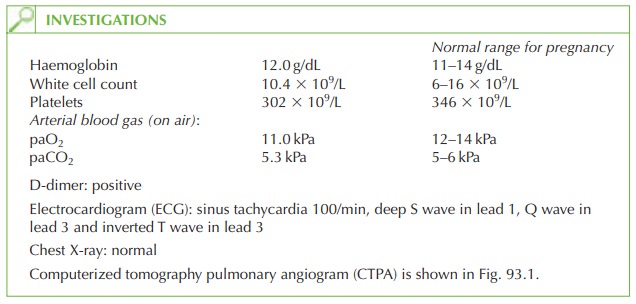
Chapter: Case Study in Obstetrics and Gynaecology: Peripartum Care and Obstetric Emergencies
Case Study Reports: Breathlessness in Pregnancy
History
A 42-year-old woman is referred
by her general practitioner with breathlessness for the past 3 days. She is 34 weeks pregnant
in her third pregnancy. Prior to this she has had an emer- gency Caesarean section for abnormal cardiotocograph in labour,
followed by a 7-week miscarriage.
In this pregnancy she was seen
by the obstetric consultant to discuss
plans for delivery, and is hoping for a vaginal
delivery. Ultrasound scans
and blood tests
have been normal. Her booking blood pressure was
138/80 mmHg and has remained stable during the pregnancy.
She describes her shortness of breath starting
while she was at work and slightly
worsen- ing since. She felt particularly breathless when she ran to catch a bus on her way home
yesterday. She has some left-sided chest pain on breathing in. There is no cough
or haemoptysis. She has
had no previous episodes. She has
not noticed any
calf pain but
has left leg swelling and some back pain.
Examination
The body mass
index is 28 kg/m2. The
woman does not
look obviously unwell.
Blood pre- ssure is 127/78 mmHg
and heart rate
98/min. Oxygen saturation is 96 per
cent on air.
On examination of the chest there
is a systolic murmur and no added
sounds. Chest expan- sion is normal but
the woman reports
pain on taking
a deep breath.
The chest is resonant
to percussion and
chest sounds are
normal except for
a pleural rub
on the left.
The left leg is
generally swollen but no redness
or tenderness is apparent.
Questions
·
What is the diagnosis?
·
What further imaging is required?
·
How
would you manage
this woman in the immediate term, during delivery
and postnatally?
ANSWER
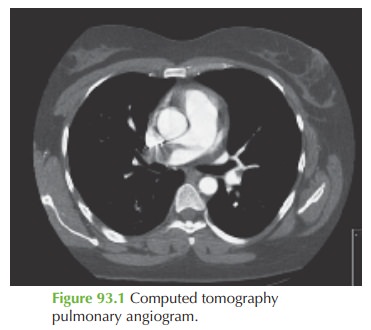
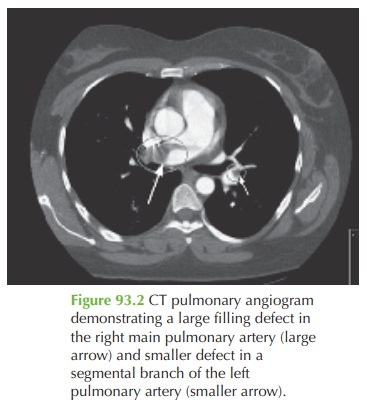
The diagnosis is of pulmonary
embolism (PE). The shortness and breath and pleuritic chest pain are classic features, and the
ECG and blood gas analysis support the diagnosis. D-dimer is commonly raised in
pregnancy but also supports the diagnosis. The CTPA demonstrates a large
filling defect within
the right pulmonary artery and a smaller filling defect in the left segmental
pulmonary artery, consistent with blood clots
(pulmonary embolism). These findings
are illustrated by the arrows
in Fig. 93.2.
Venous thromboembolism (VTE)
is the leading cause of direct deaths
in the Confidential Enquiry into Maternal and Child Health,
accounting for death
in 1.2 per
100 000 mater- nities. Non-fatal VTE occurs in approximately 60 in 10 000 pregnancies, and there may be
many more unrecognized cases. Pregnancy itself is a risk factor
because of the hyper-
oestrogenic state, the
altered blood viscosity and obstruction to venous blood
flow by the gravid uterus.
Further imaging
There is no clinical evidence of calf ileofemoral deep vein thrombosis, but generalized leg swelling and back pain
are suspicious of an ileofemoral thrombosis. If this
is confirmed, which may require Doppler
ultrasound or magnetic
resonance imaging (or if she develops
recurrent PE despite anticoagulation), then liaison with a vascular
team should be consid-
ered regarding the possibility of insertion of a vena caval filter.
Management
As with non-pregnant patients, anticoagulation is the mainstay
of treatment. Warfarin
is contraindicated in the first trimester of pregnancy but may safely
be given from 12 to 36
weeks. However it can cause difficulties with excessive bleeding
if it is not stopped
early enough before delivery
and it can be difficult
to achieve stable international normalized ratio levels. Therefore low-molecular-weight heparin
has become the treatment of choice
in pregnancy as it is simple to administer, relatively easy to reverse
in the emergency situ-
ation, does not require monitoring, and is safe.
At delivery the heparin should
ideally be discontinued 12 h before
delivery and recom- menced immediately following
delivery. Similarly an epidural or spinal anaesthetic should not be administered immediately after a heparin
dose.
Postnatally some women
change to warfarin, which is now known to be safe with breast- feeding, while others continue
low-molecular-weight heparin.
A large proportion of VTE occurs
postnatally, so anticoagulation should be continued for 6 weeks to 3 months
in the puerperium.
Graduated elastic compression stocking should be worn from the time of diagnosis until at least 6 weeks following delivery, to reduce
the risk of the post-thrombotic syndrome (chronic leg pain, swelling and ulceration).
Postnatal investigation for
inherited (e.g. protein C or S deficiency) or acquired
(e.g. anti- phospholipid
syndrome) thrombophilia is appropriate,
as is anticoagulation throughout any
subsequent pregnancy.
Related Topics