Chapter: Case Study in Obstetrics and Gynaecology: Peripartum Care and Obstetric Emergencies
Case Study Reports: Perineal Tear
PERINEAL TEAR
History
A
woman has just delivered her second baby on the labour ward.
She is 37 years old and
had a previous premature delivery
at 34 weeks. In this pregnancy she went into sponta-
neous labour at 38 weeks after an uncomplicated pregnancy.
The
symphysiofundal height was
consistent with dates
until 37 weeks
when the midwife measured it as 41 cm.
However, before an ultrasound scan
for growth and
liquor volume could be arranged the woman went into spontaneous labour.
At
the time of admission she was 5 cm dilated
and spontaneous rupture
of membranes occurred soon after. The baby was delivered 30 min later in the direct occipitoanterior position.
The
placenta was delivered by controlled cord
traction, after which
the midwife noticed
a perineal tear. The tear extended
from the introitus in the midline
and she could
see torn muscle fibres
suggestive of the torn ends of the external anal sphincter. She has called
you to review the patient.
Questions
·
What is the likely diagnosis?
·
What factors predispose to this condition?
·
How would you manage this patient?
Answer:
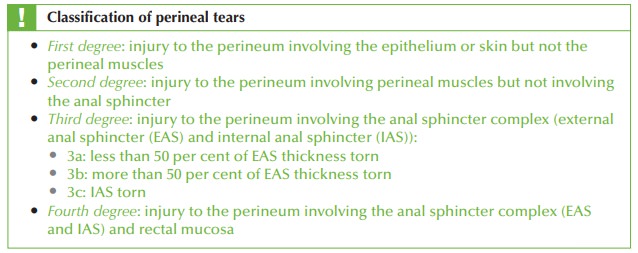
The history suggests a third-degree
tear
Risk factors
Third-degree tears occur in 2–4 per
cent of women with the following conditions:
·
birthweight over 4 kg
·
persistent occipitoposterior position
·
nulliparity
·
induction of labour
·
epidural
·
second stage of labour lasting more than 1 h
·
episiotomy
·
forceps delivery.
Third-degree tear diagnosis depends
on the vigilance of the person inspecting a tear and may
easily be missed.
This has far-reaching consequences, as failure
to perform adequate primary repair may increase
the chance of longer-term faecal
incontinence.
Management
The woman should be transferred to theatre for repair. This enables adequate
analgesia (spinal or epidural), good exposure, good lighting and availability of appropriate
instruments.
The tear should be repaired in
layers:
·
rectal mucosa (if involved)
·
internal anal sphincter (if involved)
·
external anal sphincter
·
perineal muscle
·
vaginal epithelium
·
perineal skin.
Broad-spectrum antibiotics should be administered to prevent
infection from possible contamination by bowel
organisms.
Laxatives should
be administered to prevent constipation that might compromise the repair.
Adequate postoperative
analgesia is needed.
The
woman should not generally be discharged until
she has opened
her bowels.
A
follow-up appointment should
be made after
approximately 6 weeks
to ensure that the
woman has no significant bowel
symptoms and to refer on to a colorectal specialist if she has.
Elective Caesarean section should be discussed as a possibility for any subsequent deliveries.
Related Topics