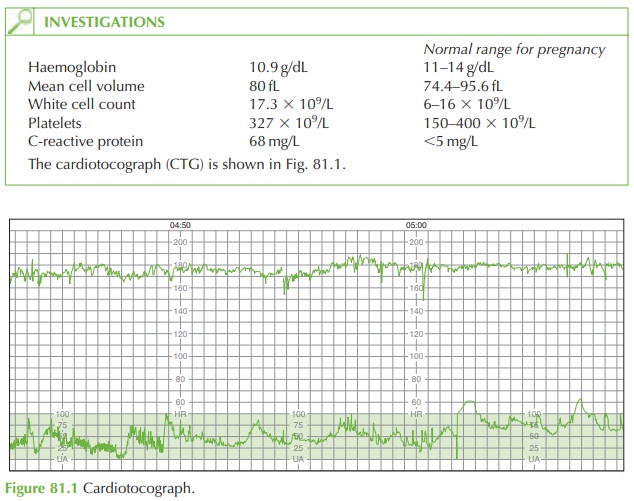
Chapter: Case Study in Obstetrics and Gynaecology: Peripartum Care and Obstetric Emergencies
Case Study Reports: Pain and Fever in Pregnancy
PAIN AND FEVER IN PREGNANCY
History
A
woman aged 26 years is referred by her general
practitioner. She is 36 weeks’
gestation in her fourth pregnancy, having had one miscarriage and two term vaginal deliveries.
In
this pregnancy she has been seen twice
in the day assessment unit,
the first time at 31 weeks for an episode
of vaginal bleeding
for which no cause was attributed. The second
time was at 35 weeks
after she awoke
with damp bed sheets. No liquor had been detected on speculum examination at the time and she was discharged. For the last 2 days she has been
feeling generally unwell with a fever, decreased
appetite and a headache as well as abdominal discomfort. She reports
the baby moving
less than normal
for the last
few days, with approximately
8–10 movements per day.
She
has not noticed any vaginal
bleeding but her discharge has been more than normal and there is an offensive odour to it.
Examination
Her
temperature is 37.8°C,
blood pressure 106/68
mmHg and heart
rate 109/min. On abdominal palpation symphysiofundal height
is 34 cm and the fetus is cephalic with 3/5
palpable. There is generalized uterine
tenderness and irritability. On speculum examina- tion the cervix is closed and
a green/grey discharge is seen within
the vagina.
Questions
·
What is the diagnosis?
·
How should this woman be managed?
Answer:
The
diagnosis is of chorioamnionitis secondary
to prolonged preterm
rupture of mem- branes. Although spontaneous rupture
of membranes was not confirmed at the previous attendance at 35 weeks, it seems probable that in fact this did occur at that time. Ascending organisms have thus
colonized the uterus
and resulted in infection. The
result is a maternal
systemic reaction causing
her symptoms: tachycardia, tenderness, leuco-
cytosis, and raised C-reactive protein.
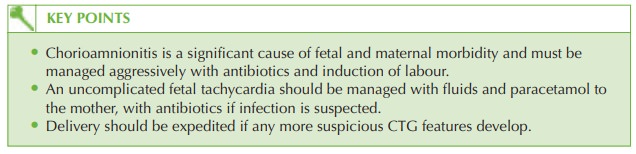
The fetus is also affected as shown
by the fetal tachycardia.
Chorioamnionitis is a significant cause of both fetal and maternal morbidity and mortal- ity, and should
be treated as an obstetric emergency.
Management should be instigated
immediately. Initial microbial specimens should be obtained from high vaginal swab and maternal
blood cultures.
Intravenous broad-spectrum
antibiotic should be commenced to cover both anaerobic and aerobic organisms. Intravenous fluids should be commenced
to counter the effects of vasodilatation and pyrexia,
and because the woman is unable to drink adequately. Paracetamol should
be given regularly for the pyrexia
and abdominal discomfort.
The
baby needs delivery
by induction of labour – women with chorioamnionitis often labour rapidly. Risks of Caesarean section
in the presence of infection are significant in terms
of bleeding, uterine
atony and disseminated intravascular coagulopathy. However continuous CTG should be employed and immediate Caesarean
section performed if it
deteriorates.
Steroids (to prevent potential respiratory distress syndrome) are contraindicated in this
woman as they may increase
the severity of infection.
After delivery, the baby
will need to be reviewed by the paediatrician and given a septic
screen and course of intravenous antibiotics.
Related Topics