Chapter: Case Study in Obstetrics and Gynaecology: Peripartum Care and Obstetric Emergencies
Case Study Reports: Headache in Pregnancy
HEADACHE IN PREGNANCY
History
A
17-year-old girl is admitted to the labour
ward by ambulance because of a severe
headache and reduced fetal movements. This is her
first pregnancy. She
did not discover she was pregnant until
very late and was uncertain of her last menstrual period
date so was dated
by ultrasound scan
at 23 weeks. According to that scan
she is now
37 weeks.
When she was first
booked in the antenatal clinic
her blood pressure
was 120/68 mmHg and
urinalysis negative. The blood pressure
was last checked
1 week ago and was 132/74 mmHg and urine
was negative again.
Booking blood tests
were all normal.
This morning she woke with a frontal headache
which has persisted despite paracetamol.
She says that her vision
is a bit blurred but she cannot
be more specific
about this. She also
reports nausea and
epigastric discomfort, but
has not vomited. She denies leg
or fin- ger swelling.
Examination
The
blood pressure is 164/106 mmHg. This is repeated twice at 15 min intervals
and is found to be 160/110 mmHg and 164/112 mmHg. She is apyrexial and her heart rate is 83/min. Her face is minimally swollen
and fundoscopy is normal. Cardiac
and respiratory examinations are
normal. Abdominally she
is tender in the epigastrium and beneath the right costal margin, but the uterus
is soft and non-tender. The fetus is cephalic and 3/5
palpable.
The
legs and fingers
are mildly oedematous and lower limb reflexes are very brisk,
with clonus.
Questions
·
What is the diagnosis?
·
How would you manage this patient?
Answer:
The
woman has pre-eclampsia with rapid onset
and severity of symptoms and
signs sug- gesting severe
or ‘fulminant’ disease.
She is at high risk of developing eclampsia.
The
headache and visual disturbance are typical features
of cerebral oedema;
the right upper quadrant
pain of subcapsular liver swelling and the proteinuria occurs from renal involvement.
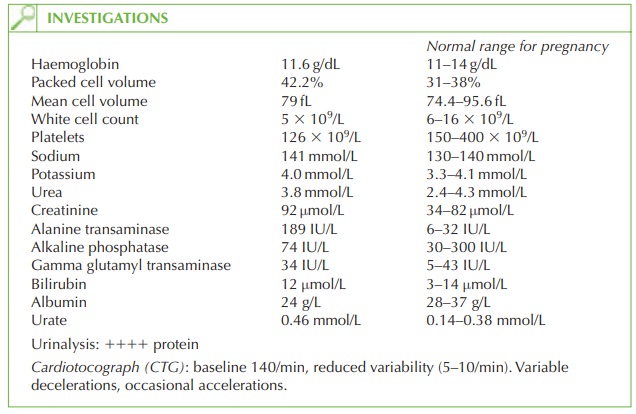
The blood tests show typical
features of severe pre-eclampsia:
·
elevated liver transaminases
·
elevated urate
·
elevated creatinine.
The
platelet count is at the lower end of the normal range
for pregnancy and if reduced further, with raised bilirubin would suggest development of HELLP syndrome (haemoly- sis, elevated liver enzymes and low platelets).
Management
This is an obstetric
emergency and the senior midwife,
anaesthetist and senior obstetrician
should be informed immediately. The only definitive treatment for pre-eclampsia is deliv- ery of the baby, but
the maternal status
must be stabilized first. In this
case she should
be admitted and have an intravenous cannula inserted. Blood
should be sent for coagulation and for group and
save. A urinary
catheter should be inserted and
fluid input and
output carefully monitored for oliguria as a sign of impending renal failure.
In
pre-eclampsia although the
extracellular fluid is increased (third
space), the intravas- cular volume is generally depleted, so fluid
input should be managed carefully with the help of an anaesthetist, balancing adequate renal
perfusion with the
risk of overload and pulmonary oedema. Where the urine output is decreased, a central venous line may be
needed for more accurate assessment of volume status.
The
woman should be given an antihypertensive to reduce her blood pressure
(thus redu- cing the
risk of cerebral haemorrhage). If initial
oral antihypertensives are
not effective, a titrated intravenous infusion should
be used.
Magnesium sulphate infusion reduces
the risk of an eclamptic fit in women
with severe pre-eclampsia and
should be commenced.
The
CTG shows reduced
variability and occasional variable decelerations. This suggests
that the reduced fetal movements may be due
to fetal distress, probably from uteroplacen- tal insufficiency. Caesarean section
would therefore be the mode
of delivery of choice, but only when the maternal
blood pressure is under control
and the coagulation screen result is available.
Postnatally the condition may
not improve for
48 h or more, and
the woman should
be nursed in a high-dependency setting
until the blood
pressure is under
control, renal out- put is normal, symptoms have settled and
blood results are
returning to normal.
Related Topics