Chapter: Medical Surgical Nursing: Management of Patients With Urinary Disorders
Nursing Process: The Patient Undergoing Urinary Diversion Surgery
NURSING
PROCESS: THE PATIENT UNDERGOING URINARY DIVERSION SURGERY
Preoperative Assessment
The
following are key preoperative nursing assessment concerns:
· Cardiopulmonary function
assessments are performed be-cause patients undergoing cystectomy (excision of
the uri-nary bladder) are often older people who may not be able to tolerate a
lengthy, complex surgical procedure.
· A nutritional status
assessment is important because of pos-sible poor nutritional intake related to
underlying health problems.
· Learning needs are
assessed to evaluate the patient’s and the family’s understanding of the
procedure and the changes in physical structure and function that result from
the surgery. The patient’s self-concept and self-esteem are assessed, in
addition to methods for coping with stress and loss. The pa-tient’s mental
status, manual dexterity and coordination, and preferred method of learning are
noted because they will affect postoperative self-care.
Preoperative Nursing Diagnoses
Based
on the assessment data, the preoperative nursing diagnoses for the patient
undergoing urinary diversion surgery may include the following:
· Anxiety related to
anticipated losses associated with the sur-gical procedure
· Imbalanced nutrition,
less than body requirements related to inadequate nutritional intake
·
Deficient knowledge about the surgical procedure
and post-operative care
Preoperative Planning and Goals
The
major goals for the patient may include relief of anxiety, im-proved
preoperative nutritional status, and increased knowledge about the surgical
procedure, expected outcomes, and post-operative care.
Preoperative Nursing Interventions
RELIEVING ANXIETY
The
threat of cancer and removal of the bladder create fears related to body image
and security. The patient faces problems in adapt-ing to an external appliance,
a stoma, a surgical incision, and al-tered toileting habits. The male patient
must also adapt to sexual impotency. (A penile implant is considered if the
patient is a can-didate for the procedure.) Women also fear altered appearance,
body image, and self-esteem. A supportive approach, both physi-cal and
psychosocial, is needed and includes assessing the patient’s self-concept and
manner of coping with stress and loss; helping the patient to identify ways to
maintain his or her lifestyle and in-dependence with as few changes as
possible; and encouraging the patient to express fears and anxieties about the
ramifications of the upcoming surgery. A visitor from the Ostomy Visitation
Program of the American Cancer Society can provide emotional support and make
adaptation easier both before and after surgery.
ENSURING ADEQUATE NUTRITION
In
addition to cleansing the bowel to minimize fecal stasis, decom-press the
bowel, and minimize postoperative ileus, a low-residue diet is prescribed and
antibiotic medications are administered to re-duce pathogenic flora in the
bowel and to reduce the risk of infec-tion. Because the patient undergoing a
urinary diversion procedure for cancer may be severely malnourished due to the
tumor, radia-tion enteritis, and anorexia, enteral or parenteral nutrition may
be prescribed to promote healing. Adequate preoperative hydration is imperative
to ensure urine flow during surgery and to prevent hypovolemia during the
prolonged surgical procedure.
EXPLAINING SURGERY AND ITS EFFECTS
An
enterostomal therapist is invaluable in preoperative teaching and in planning
postoperative care. Explanations of the surgical procedure, the appearance of
the stoma, the rationale for preoper-ative bowel preparation, the reasons for
wearing a collection device, and the anticipated effects of the surgery on
sexual functioning are part of patient teaching. The placement of the stoma
site is planned preoperatively with the patient standing, sitting, or lying
down to locate the stoma away from bony prominences, skin creases, and fat
folds. The stoma should also be placed away from old scars, the umbilicus, and
the belt line.
For
ease of self-care, the patient must be able to see and reach the site
comfortably. The site is marked with indelible ink so that it can be located
easily during surgery. The patient is assessed for allergies or sensitivity to
tape or adhesives. (Patch testing of cer-tain appliances may be necessary
before the ostomy equipment is selected. This is particularly important if the
patient may be or is allergic to latex.) It may be helpful to have the patient
practice wearing an appliance partially filled with water before surgery
(Krupski & Theodorescu, 2001).
Preoperative Evaluation
To
measure the effectiveness of care, the nurse evaluates the pre-operative
patient’s anxiety level and nutritional status as well as his or her knowledge
and expectations of surgery.
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1) Exhibits reduced anxiety
about surgery and expected losses
a)
Verbalizes fears with health care team and family
b)
Expresses positive attitude about outcome of
surgery
2) Exhibits adequate
nutritional status
a)
Maintains adequate intake before surgery
b)
Maintains body weight
c)
States rationale for enteral or parenteral
nutrition if needed
d)
Exhibits normal skin turgor, moist mucous
membranes, adequate urine output, and absence of excessive thirst
3) Demonstrates knowledge
about the surgical procedure and postoperative course
a)
Identifies limitations expected after surgery
b)
Discusses expected immediate postoperative
environ-ment (tubes, machines, nursing surveillance)
c)
Practices deep breathing, coughing, and foot
exercises
Postoperative Assessment
The
role of the nurse in the immediate postoperative period is to prevent
complications and to assess the patient carefully for any signs and symptoms of
complications. The catheters and any drainage devices are monitored closely.
Urine volume, patency of the drainage system, and color of the drainage are
assessed. A sud-den decrease in urine volume or increase in drainage is
reported promptly to the physician because these may indicate obstruction of
the urinary tract, inadequate blood volume, or bleeding. In ad-dition, the
patient’s needs for pain control are assessed (Colwell, Goldberg & Cramel,
2001).
Postoperative Diagnosis
NURSING DIAGNOSES
Based
on the assessment data, the major postoperative nursing di-agnoses for the
patient following urinary diversion surgery may include the following:
· Risk for impaired skin
integrity related to problems in man-aging the urine collection appliance
· Acute pain related to
surgical incision
· Disturbed body image
related to urinary diversion
· Potential for sexual
dysfunction related to structural and physiologic alterations
· Deficient knowledge
about management of urinary function
Collaborative Problems/ Potential Complications
Potential
complications may include the following:
· Peritonitis due to
disruption of anastomosis
· Stomal ischemia and
necrosis due to compromised blood supply to stoma
· Stoma retraction and
separation of mucocutaneous border due to tension or trauma
Postoperative Planning and Goals
The
major goals for the patient may include maintaining peri-stomal skin integrity,
relieving pain, increasing self-esteem, de-veloping appropriate coping
mechanisms to accept and deal with altered urinary function and sexuality,
increasing knowledge about management of urinary function, and preventing
poten-tial complications (Krupski & Theodorescu, 2001; O’Shea, 2001).
Postoperative Nursing Interventions
Postoperative
management focuses on monitoring urinary func-tion, preventing postoperative
complications (infection and sep-sis, respiratory complications, fluid and
electrolyte imbalances, fistula formation, and urine leakage), and promoting
patient comfort. Catheters or drainage systems are observed, and urine output
is monitored carefully. A nasogastric tube is inserted dur-ing surgery to
decompress the GI tract and to relieve pressure on the intestinal anastomosis.
It is usually kept in place for several days after surgery. As soon as bowel
function resumes, as indi-cated by bowel sounds, the passage of flatus, and a soft
abdomen, oral fluids are permitted. Until that time, intravenous fluids and
electrolytes are administered. The patient is assisted to ambulate as soon as
possible to prevent complications of immobility.
MAINTAINING PERISTOMAL SKIN INTEGRITY
Strategies
to promote skin integrity begin with reducing and con-trolling those factors
that increase the patient’s risk for poor nu-trition and poor healing. As
indicated previously, meticulous skin care and management of the drainage
system are provided by the nurse until the patient can manage them and is
comfortable doing so. Care is taken to keep the drainage system intact to
pro-tect the skin from exposure to drainage. Supplies must be readily available
to manage the drainage in the immediate postoperative period. Consistency in
implementing the skin care program throughout the postoperative period will
result in maintenance of skin integrity and patient comfort. Additionally,
maintenance of skin integrity around the stoma will enable the patient and
family to adjust more easily to the alterations in urinary function and will
help them to learn skin care techniques.
RELIEVING PAIN
Analgesic
medications are administered liberally postoperatively to relieve pain and
promote comfort, thereby allowing the patient to turn, cough, and do
deep-breathing exercises. Patient-controlled analgesia and administration of
analgesic agents regularly around the clock are two options that may be used to
ensure adequate pain relief. A pain-intensity scale is used to evaluate the adequacy
of the medication and the approach to pain management.
IMPROVING BODY IMAGE
The
patient’s ability to cope with the changes associated with the surgery depends
to some degree on his or her body image and self-esteem before the surgery and
the support and reaction of others. Allowing the patient to express concerns
and anxious feelings can help, especially in adjusting to the changes in
toileting habits. The nurse can also help improve the patient’s self-concept by
teaching the skills needed to be independent in managing the urinary drainage
devices. Education about ostomy care is conducted in a private setting to
encourage the patient to ask questions without fear of embarrassment.
Explaining why the nurse must wear gloves when performing ostomy care can
prevent the patient from mis-interpreting the use of gloves as a sign of
aversion to the stoma.
EXPLORING SEXUALITY ISSUES
Patients
who experience altered sexual function as a result of the surgical procedure
may mourn for this loss. Encouraging the patient and partner to share their
feelings about this loss with each other and acknowledging the importance of
sexual function and expression may encourage the patient and partner to seek
sexual counseling and to explore alternative ways of expressing sexual-ity. A
visit from another “ostomate” who is functioning fully in society and family
life may also assist the patient and family in recognizing that full recovery
is possible.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Complications
are not unusual because of the complexity of the surgery, the underlying reason
(cancer, trauma) for the urinary diversion procedure, and the patient’s
frequently less-than-optimal nutritional status. Complications may include the
usual post-operative complications (eg, respiratory problems, such as
atelec-tasis, fluid and electrolyte imbalances) as well as breakdown of the
anastomoses, sepsis, fistula formation, fecal or urine leakage, and skin
irritation. If these occur, the patient will remain hospitalized for an extended
length of time and will probably require parenteral nutrition, GI decompression
by means of nasogastric suction, and further surgery. The goals of management
are to establish drainage, provide adequate nutrition for healing to occur, and
prevent sepsis.
Peritonitis
Peritonitis
can occur postoperatively if urine leaks at the anasto-mosis. Signs and
symptoms include abdominal pain and disten-tion, muscle rigidity with guarding,
nausea and vomiting, paralytic ileus (absence of bowel sounds), fever, and
leukocytosis.
Urine
output must be monitored closely because a sudden de-crease in amount with a
corresponding increase in drainage from the incision or drains may indicate
urine leakage. In addition, the urine drainage device is observed for leakage.
The pouch is changed if a leak is observed. Small leaks in the anastomosis may
seal them-selves, but surgery may be needed for larger leaks.
Vital
signs (blood pressure, pulse and respiratory rates, temper-ature) are
monitored. Changes in vital signs, as well as increasing pain, nausea and
vomiting, and abdominal distention, are reported to the physician and may
indicate peritonitis.
Stomal Ischemia and Necrosis
The
stoma is monitored because stomal ischemia and necrosis can result from tension
on the mesentery blood vessels, twisting of the bowel segment (conduit) during
surgery, or arterial insufficiency. The new stoma must be inspected at least
every 4 hours to assess the adequacy of its blood supply. The stoma should be
red or pink. If the blood supply to the stoma is compromised, the color changes
to purple, brown, or black. These changes are reported immediately to the
physician. The physician or enterostomal therapist may insert a small,
lubricated tube into the stoma and shine a flashlight into the lumen of the
tube to assess for super-ficial ischemia or necrosis. A necrotic stoma requires
surgical intervention. If the ischemia is superficial, the dusky stoma is
observed and may slough its outer layer in several days.
Stomal Retraction and Separation
Stoma
retraction and separation of the mucocutaneous border can occur as a result of
trauma or tension on the internal bowel segment used for creation of the stoma.
In addition, mucocuta-neous separation can occur if the stoma does not heal as
a result of accumulation of urine on the stoma and mucocutaneous bor-der. Using
a collection drainage pouch with an antireflux valve is helpful because the
valve prevents urine from pooling on the stoma and mucocutaneous border.
Meticulous skin care to keep the area around the stoma clean and dry promotes
healing. If a separation of the mucocutaneous border occurs, surgery is not
usually needed. The separated area is protected by applying karaya powder,
stoma adhesive paste, and a properly fitted skin barrier and pouch. By
protecting the separation, healing is promoted. If the stoma retracts into the
peritoneum, surgical intervention is mandatory.
If
surgery is needed to manage these complications, the nurse provides
explanations to the patient and family. The need for ad-ditional surgery is
usually perceived as a setback by the patient and family. Emotional support of
the patient and family is pro-vided along with physical preparation of the
patient for surgery.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
A
major postoperative objective is to assist the patient to achieve the highest
level of independence and self-care possible. The primary nurse and
enterostomal therapist work closely with the patient and family to instruct and
assist them in all phases of managing the ostomy. Adequate supplies and
complete instruc-tion are necessary to enable the patient and a family member
to develop competence and confidence in their skills. Written and verbal
instructions are provided, and the patient is encouraged to contact the nurse
or physician with follow-up questions. Follow-up telephone calls from the nurse
to the patient and family after discharge may provide added support and provide
another op-portunity to answer their questions. Follow-up visits and
re-inforcement of correct skin care and appliance management techniques also
promote skin integrity. Specific techniques for managing the appliance are
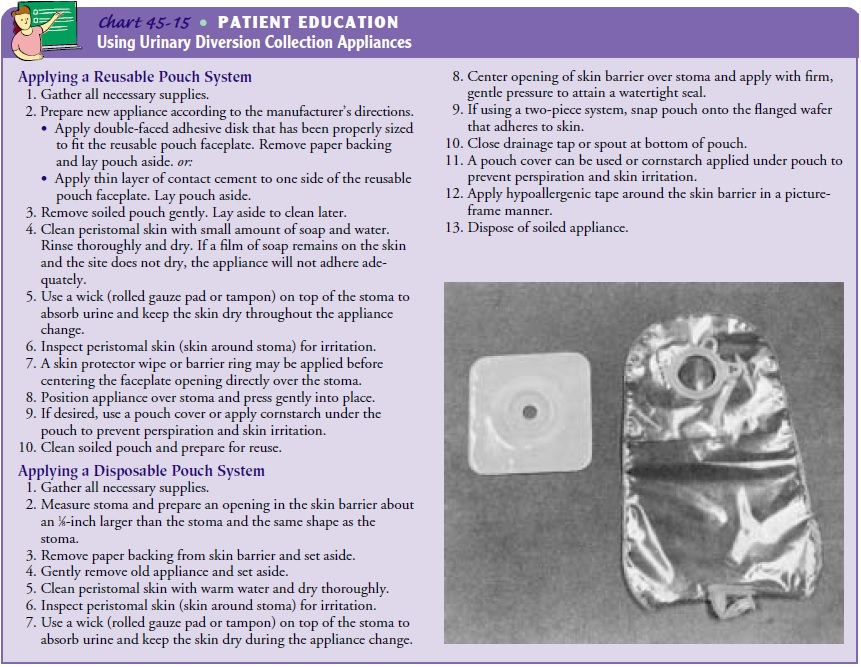
described in Chart 45-15.
The
patient is encouraged to participate in decisions regard-ing the type of
collecting appliance and the time of day to change the appliance. The patient
is assisted and encouraged to look at and touch the stoma early to overcome any
fears. The patient and family need to know the characteristics of a normal
stoma, as follows:
· Pink and moist, like the
inside of the mouth
· Insensitive to pain
because it has no nerve endings
· Vascular and may bleed
when cleaned
Additionally,
if a segment of the GI tract was used to create the urinary diversion, mucus
may be visible in the urine. By learn-ing what is normal, the patient and
family become familiar with what signs and symptoms they should report to the
physician or nurse and what problems they can handle themselves.
Information
provided to the patient and the extent of in-volvement in self-care are
determined by the patient’s physical re-covery and ability to accept and
acquire the knowledge and skill needed for independence. Verbal and written
instructions are provided, and the patient is given the opportunity to practice
and demonstrate the knowledge and skills needed to manage urinary drainage.
Continuing Care
Follow-up
care is essential to determine how the patient has adapted to the body image
changes and lifestyle adjustments. Vis-its from a home care nurse are important
to assess the patient’s adaptation to the home setting and management of the
ostomy. Teaching and reinforcement may assist the patient and family to cope
with altered urinary function. It is also necessary to assess for long-term
complications that may occur, such as pouch leakage or rupture, stone
formation, stomal stenosis, deterioration in renal function, or incontinence
(Baker, 2001).
The
following procedures are recommended for patients with
continent urinary
diversion: pouch-o-gram (x-rays taken after
radioactive agent is
instilled into the pouch) between 3 and
6
months, 9 and 12 months, 24 months, then every other year; renal function tests
(BUN, serum creatinine) 1 month, 3 months, 6 months, then twice yearly; and
pouchoscopy (endoscopic exam-ination of the pouch) every year starting 5 to 7
years after surgery (Colwell, Goldberg & Cramel, 2001). The patient who has
had surgery for carcinoma should have a yearly physical examination and chest
x-ray to assess for metastases. In addition, the patient and family are
reminded of the importance of participating in health promotion activities and
recommended health screening.
Long-term
monitoring for anemia is performed to identify vi-tamin B deficiency, which may
occur when a significant portion of the terminal ileum is removed. This may
take several years to develop and can be treated with vitamin B injections. The
patient and family are informed of the United Ostomy Association and any local
ostomy support groups to provide ongoing support, assistance, and education.
Postoperative Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1) Maintains skin integrity
a)
Maintains intact peristomal skin and demonstrates
skill in managing drainage system and appliance
b)
Reports absence of pain or discomfort in peristomal
area
c)
States actions to take if skin excoriation occurs
2) Exhibits increased
knowledge about managing urinary function
a)
Participates in managing urinary system and skin
care
b)
Verbally describes anatomic alteration due to
surgery
c)
Revises daily routine to accommodate urinary
drainage management
d)
Identifies potential problems, reportable signs and
symptoms, and subsequent measures to take
3) Exhibits improved
self-concept as evidenced by the fol-lowing:
a)
Voices acceptance of urinary diversion, stoma, and
appliance
b)
Demonstrates increasingly independent self-care,
in-cluding hygiene and grooming
c)
States acceptance of support and assistance from
family members, health care providers, and other ostomates
4) Copes with sexuality
issues
a)
Verbalizes concern about possible alterations in
sexual-ity and sexual function
b)
Reports discussion of sexual concerns with partner
and appropriate counselor
5) Demonstrates knowledge
needed for self-care
a)
Performs self-care and proficient management of
uri-nary diversion and appliance
b)
Asks questions relevant to self-management and
pre-vention of complications
c)
Identifies signs and symptoms needing care from
physi-cian or other health care providers
6) Absence of complications
as evidenced by the following:
a)
Reports absence of pain or tenderness in abdomen
b)
Has temperature within normal range
c)
Reports no urine leakage from incision or drains
d)
Has urine output within desired volume limits
e)
Maintains stoma that is red or pink, moist, and
appro-priately “budded”
f)
Has intact and healed stomal border
Related Topics