Chapter: Medical Surgical Nursing: Management of Patients With Urinary Disorders
Kidney Transplantation
Kidney Transplantation
Kidney
transplantation has become the treatment of choice for most patients with ESRD.
During the past 40 years, more than 380,000 kidney transplantations have been
performed world-wide, and more than 174,000 have been performed in the United
States. This number includes over 10,000 kidney-pancreas trans-plantations. In
January 2003 there were almost 54,000 persons on the waiting list for kidney
transplantation (http://www.unos.org., December 25, 2002). Patients
choose kidney transplantation for various reasons, such as the desire to avoid
dialysis or to improve their sense of well-being and the wish to lead a more
normal life. Additionally, the cost of maintaining a successful transplantation
is one-third the cost of treating a dialysis patient.
Kidney
transplantation involves transplanting a kidney from a living donor or human
cadaver to a recipient who has ESRD (Chart 45-9). Kidney transplants from
well-matched living donors who are related to the patient (those with
compatible ABO and HLA antigens) are slightly more successful than those from
ca-daver donors. The success rate increases if kidney transplanta-tion from a
living donor is performed before dialysis is initiated (Mange, Joffe &
Feldman, 2001). Due to the overwhelming numbers of persons on kidney transplant
waiting lists, new tech-niques for matching nonrelated living donors are being
devel-oped (Gridelli & Remuzzi, 2000).
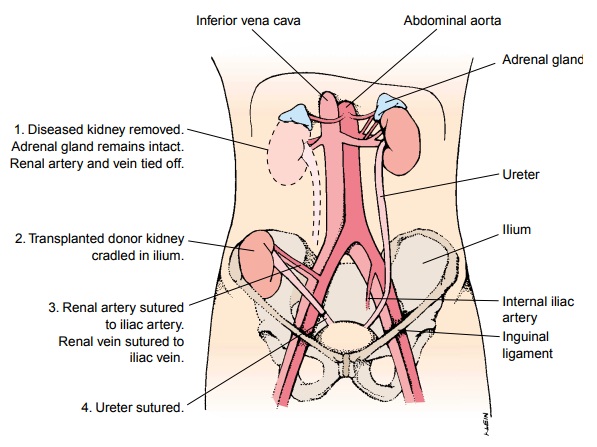
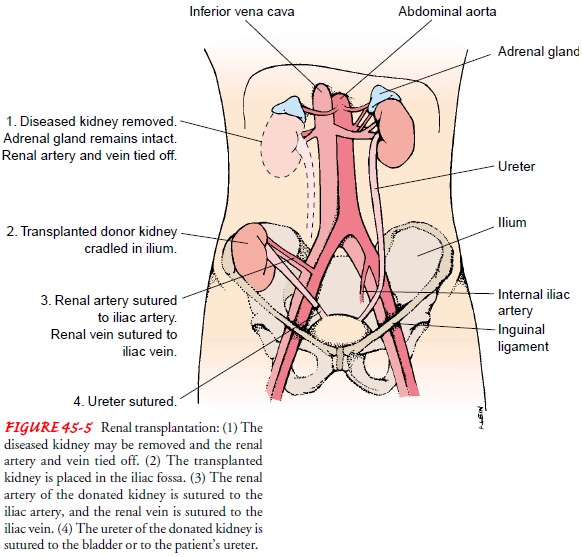
A
nephrectomy of the patient’s own native kidneys may be performed before
transplantation. The transplanted kidney is placed in the patient’s iliac fossa
anterior to the iliac crest. The ureter of the newly transplanted kidney is
transplanted into the bladder or anastomosed to the ureter of the recipient
(Fig. 45-5).
PREOPERATIVE MANAGEMENT
Preoperative
management goals include bringing the patient’s metabolic state to a level as
close to normal as possible, making sure that the patient is free of infection,
and preparing the patient for surgery and the postoperative course.
Medical Management
A
complete physical examination is performed to detect and treat any conditions
that could cause complications after transplanta-tion. Tissue typing, blood
typing, and antibody screening are per-formed to determine compatibility of the
tissues and cells of the donor and recipient. Other diagnostic tests must be
completed to identify conditions requiring treatment before transplantation.
The lower urinary tract is studied to assess bladder neck function and to
detect ureteral reflux.
The
patient must be free of infection at the time of renal trans-plantation because
after surgery the patient will receive medications to prevent transplant
rejection. These medications suppress the immune response, leaving the patient
immunosuppressed and at risk for infection. Therefore, the patient is evaluated
and treated for any infections, including gingival (gum) disease and dental
caries.
A
psychosocial evaluation is conducted to assess the patient’s ability to adjust
to the transplant, coping styles, social history, social support available, and
financial resources. A history of psy-chiatric illness is important to
ascertain because psychiatric con-ditions are often aggravated by the
corticosteroids needed for immunosuppression after transplantation.
Hemodialysis
is often performed the day before the scheduled transplantation procedure to
optimize the patient’s physical sta-tus if a dialysis routine had already been
established. However, it is preferable to avoid initiation of dialysis before
transplantation when a donor kidney is available (Mange et al., 2001).
Nursing Management
The
nursing aspects of preoperative care are similar to those for pa-tients
undergoing other elective abdominal surgery. Preoperative teaching can be
conducted in a variety of settings, including the outpatient preadmission area,
the hospital, or the transplantation clinic during the preliminary workup
phase. Patient teaching ad-dresses postoperative pulmonary hygiene, pain
management options, dietary restrictions, intravenous and arterial lines, tubes
(indwelling catheter and possibly a nasogastric tube), and early am-bulation.
The patient who receives a kidney from a living related donor may be concerned
about the donor and how the donor will tolerate the surgical procedure.
Most
patients have been on dialysis for months or years before transplantation. Many
have waited months to years for a kidney transplant and are anxious about the
surgery, possible rejection, and the need to return to dialysis. Helping the
patient to deal with these concerns is part of the nurse’s role in preoperative
manage-ment, as is teaching the patient about what to expect after surgery.
POSTOPERATIVE MANAGEMENT
The
goal of care is to maintain homeostasis until the transplanted kidney is
functioning well. The patient whose kidney functions immediately has a more
favorable prognosis than the patient whose kidney does not.
Immunosuppressive Therapy
The
survival of a transplanted kidney depends on the ability to block the body’s
immune response to the transplanted kidney. To overcome or minimize the body’s
defense mechanism, immuno-suppressant agents such as azathioprine (Imuran),
corticosteroids (prednisone), cyclosporine, and OKT-3 (a monoclonal antibody)
are administered (Shapiro,
2000b).
Cyclosporine is available in a microemulsion
form (Neoral), which delivers the medication reliably, thus producing a
steady-state serum concentration. Tacrolimus (Prograf, formerly called FK-506) is similar to
cyclosporine and about 100 times more potent. Mycophenolate (CellCept,
RS-61433) has been approved by the U.S. Food and Drug Administration (FDA) solely
for the pre-vention of renal transplant rejection. It may be used in patients
who have failed to respond to the standard corticosteroid pulse therapy or
OKT-3. Antilymphocyte globulin is occasionally used to modify the immune
response. Leukapheresis, lymph drainage, and cyclophosphamide (Cytoxan) are
other methods of immuno-suppression, but they are rarely used.
Treatment
with combinations of these new agents has dramat-ically improved survival
rates. The newest class of agents, the first of which is sirolimus, is called
target of rapamycin (TOR) in-hibitors; these agents are used with cyclosporine
for maintenance therapy. Immunosuppressive drug therapy after kidney
transplan-tation continues to evolve (Chan, Gaston & Hariharan, 2001).
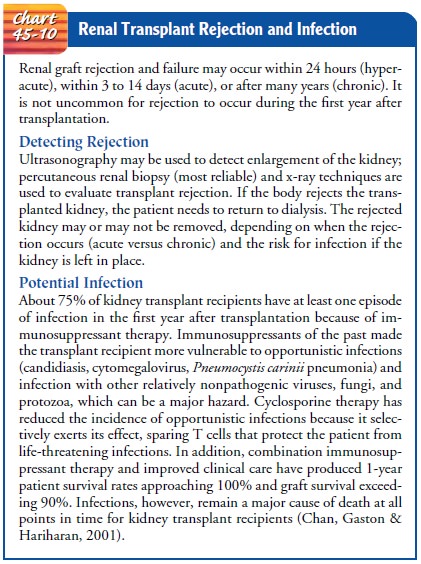
Doses
of immunosuppressant agents are gradually reduced (ta-pered) over a period of
several weeks, depending on the patient’s immunologic response to the
transplant. The patient will, how-ever, take some form of antirejection
medication for the entire time that he or she has the transplanted kidney
(Chart 45-10).
The clinical profile of neurotoxicity caused by immunosup-pression has changed. When toxic levels are reached, both cy-closporine and tacrolimus may produce a clinical spectrum that varies from tremor and acute confusional state to status epilepti-cus and major speech or language abnormalities. Coma has be-come an unusual manifestation (Baan et al., 2001; Shapiro, 2000; Wijdicks, 2001).
Postoperative Nursing Management
ASSESSING THE PATIENT FOR TRANSPLANT REJECTION
After
kidney transplantation, the nurse assesses the patient for signs and symptoms
of transplant rejection: oliguria, edema, fever, increasing blood pressure,
weight gain, and swelling or tender-ness over the transplanted kidney or graft.
Patients receiving cy-closporine may not exhibit the usual signs and symptoms
of acute rejection. In these patients, the only sign may be an asymptomatic
rise in the serum creatinine level (more than a 20% rise is con-sidered acute
rejection).
The
results of blood chemistry tests (BUN and creatinine) and leukocyte and
platelet counts are monitored closely because im-munosuppression depresses the
formation of leukocytes and platelets. The patient is closely monitored for
infection because of susceptibility to impaired healing and infection related
to immunosuppressive therapy and complications of renal failure.
Clinical
manifestations of infection include shaking chills, fever, rapid heartbeat and
respirations (tachycardia and tachypnea), and either an increase or a decrease
in WBCs (leukocytosis or leukopenia).
PREVENTING INFECTION
Infection
may be introduced through the urinary tract, the respi-ratory tract, the
surgical site, or other sources. Urine cultures are performed frequently because
of the high incidence of bacteriuria during early and late stages of
transplantation. Any type of wound drainage should be viewed as a potential
source of infection be-cause drainage is an excellent culture medium for
bacteria. Cath-eter and drain tips may be cultured when removed by cutting off
the tip of the catheter or drain (using aseptic technique) and placing the cut
portion in a sterile container to be taken to the laboratory for culture.
The
nurse ensures that the patient is protected from exposure to infection by
hospital staff, visitors, and other patients with ac-tive infections. Careful
hand hygiene is imperative; facemasks may be worn by hospital staff and
visitors to reduce the risk for transmitting infectious agents while the
patient is receiving high doses of immunosuppressants.
MONITORING URINARY FUNCTION
The
vascular access for hemodialysis is monitored to ensure pa-tency and to
evaluate for evidence of infection. After successful renal transplantation, the
vascular access device may clot, possi-bly from improved coagulation with the
return of renal func-tion. Hemodialysis may be necessary postoperatively to
maintain homeostasis until the transplanted kidney is functioning well.
A
kidney from a living donor related to the patient usually be-gins to function
immediately after surgery and may produce large quantities of dilute urine. A
kidney from a cadaver donor may un-dergo acute tubular necrosis and therefore
may not function for 2 or 3 weeks, during which time anuria, oliguria, or polyuria
may be present. During this stage, the patient may experience signifi-cant
changes in fluid and electrolyte status. Therefore, careful monitoring is
indicated. The output from the urinary catheter (connected to a closed drainage
system) is measured every hour. Intravenous fluids are administered on the
basis of urine volume and serum electrolyte levels and as prescribed by the
physician.Hemodialysis may be required if fluid overload and hyperkalemia occur
(Gridelli & Remuzzi, 2000).
ADDRESSING PSYCHOLOGICAL CONCERNS
The
rejection of a transplanted kidney remains a matter of great concern to the
patient, the family, and the health care team for many months. The fears of
kidney rejection and the complica-tions of immunosuppressive therapy (Cushing’s
syndrome, dia-betes, capillary fragility, osteoporosis, glaucoma, cataracts,
acne) place tremendous psychological stresses on the patient. Anxiety and
uncertainty about the future and difficult posttransplantation adjustment are
often sources of stress for the patient and family.
An
important nursing function is the assessment of the patient’s stress and
coping. The nurse uses each visit with the patient to de-termine if the patient
and family are coping effectively and the pa-tient is complying with the prescribed
medication regimen. If indicated or requested, the nurse refers the patient for
counseling.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
The
patient undergoing kidney transplantation is at risk for the postoperative
complications that are associated with any surgical procedure. In addition, the
patient’s physical condition may be compromised because of the complications
associated with long-standing renal failure and its treatment. Therefore,
careful assess-ment for the complications related to renal failure and those
associated with a major surgical procedure are important aspects of nursing
care. Strategies to promote surgical recovery (breath-ing exercises, early
ambulation, care of the surgical incision) are important aspects of
postoperative care.
GI
ulceration and corticosteroid-induced bleeding may occur. Fungal colonization
of the GI tract (especially the mouth) and urinary bladder may occur secondary
to corticosteroid and anti-biotic therapy. Closely monitoring the patient and
notifying the physician about the occurrence of these complications are
im-portant nursing interventions. In addition, the patient is moni-tored
closely for signs and symptoms of adrenal insufficiency if the treatment has
included use of corticosteroids.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care. The nurse
works closely with thepatient and family to be sure that they understand the
need for continuing the immunosuppressive therapy as prescribed. Addi-tionally,
the patient and family are instructed to assess for and re-port signs and
symptoms of transplant rejection, infection, or significant adverse effects of
the immunosuppressant regimen. These include decreased urine output; weight
gain; malaise; fever; respiratory distress; tenderness over the transplanted
kidney; anx-iety; depression; changes in eating, drinking, or other habits; and
changes in blood pressure readings. The patient is instructed to inform other
health care providers (eg, dentist) about the kidney transplant and the use of
immunosuppressive agents.
Continuing Care. The patient
needs to know that follow-up careafter transplantation is a lifelong necessity.
Individual verbal and written instructions are provided concerning diet,
medication, fluids, daily weight, daily measurement of urine, management of
intake and output, prevention of infection, resumption of activ-ity, and
avoidance of contact sports in which the transplanted kidney may be injured.
Because of the risk of other potential complications, the patient is followed
closely. Cardiovascular dis-ease is now the major cause of morbidity and
mortality after transplantation,
due in part to the increasing age of transplanta-tion patients. An additional
problem is possible malignancy; pa-tients receiving long-term immunosuppressive
therapy have been found to develop cancers more frequently than the general
pop-ulation. Because of the usual need for health promotion along with the
increased risks for malignancy because of immuno-suppressive therapy, the
patient is reminded of the importance of health promotion and health screening.
The
American Association of Kidney Patients is a nonprofit organization that serves
the needs of those with kidney disease. It has many helpful sugges-tions for
patients and family members learning to cope with dial-ysis and
transplantation.
Related Topics