Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Patients with Cardiovascular Disease
Hypertension
HYPERTENSION
Patients with hypertension frequently
present for elective surgical procedures. Some will have been effectively
managed, but unfortunately, many others will not have been. Hypertension is a
leading cause of death and disability in most Western societies and the most
prevalent preoperative medical abnormal-ity in surgical patients, with an
overall prevalence of 20% to 25%. Long-standing uncontrolled hyper-tension
accelerates atherosclerosis and hypertensive organ damage. Hypertension is a
major risk factor for cardiac, cerebral, renal, and vascular disease.
Complications of hypertension include
MI, con-gestive heart failure, stroke, renal failure, periph-eral occlusive
disease, and aortic dissection. The presence of left ventricular hypertrophy
(LVH) in hypertensive patients may be an important predic-tor of cardiac
mortality. However, systolic blood pressures below 180 mm Hg, and diastolic
pressures below 110 mm Hg, have not been associated with increased
perioperative risks. When patients present with systolic blood pressures
greater than 180 mm Hg and diastolic pressures greater than 110 mm Hg,
anesthesiologists face the dilemma of delaying sur-gery to allow optimization
of oral antihypertensive therapy, but adding the risk of a surgical delay
versus proceeding with surgery and achieving blood pres-sure control with
rapidly acting intravenous agents. Intravenous β-blockers can be useful to treat
preop-erative hypertension. Of note, patients with preop-erative hypertension
are more likely than others to develop intraoperative hypotension. This is
particu-larly frequent in patients treated with angiotensin receptor blockers
and/or angiotensin-converting enzyme (ACE) inhibitors.
Blood pressure measurements are affected
by many variables, including posture, time of day or night, emotional state,
recent activity, and drug intake, as well as the equipment and technique used.
A diagnosis of hypertension cannot be made by one preoperative reading, but
requires confirmation by a history of consistently elevated measurements.
Although preoperative anxiety or pain may produce some degree of hypertension
in normal patients, patients with a history of hypertension generally exhibit
greater preoperative elevations in blood pressure.
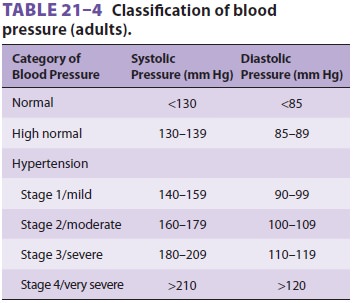
Epidemiological studies demonstrate a
direct and continuous correlation between both diastolic and systolic blood
pressures and mortality rates. The definition of systemic hypertension is
arbitrary: a consistently elevated diastolic blood pressure greater than 90 mm
Hg or a systolic pressure greater than 140 mm Hg. A common classification
scheme is listed in Table 21–4. Borderline hypertension is said to
exist when the diastolic pressure is 85–89 mm Hg or the systolic pressure is
130–139 mm Hg. Whether patients with borderline hypertension are at some
increased risk for cardiovascular complications remains unclear. Accelerated,
or severe hypertension (stage 3), is defined as a recent, sustained, and
pro-gressive increase in blood pressure, usually with dia-stolic blood
pressures in excess of 110–119 mm Hg. Renal dysfunction is often present in
such patients. Malignant hypertension is a true medical emer-gency
characterized by severe hypertension (>210/ 120 mm Hg) often associated with
papilledema and encephalopathy.
Pathophysiology
Hypertension can be either idiopathic
(essential), or, less commonly, secondary to other medical con-ditions such as
renal disease, renal artery stenosis, primary hyperaldosteronism, Cushing’s
disease, acromegaly, pheochromocytoma, pregnancy, or estrogen therapy.
Essential hypertension accountsfor 80% to 95% of cases and may be associated
with an abnormal baseline elevation of cardiac output, systemic vascular
resistance (SVR), or both. An evolving pattern is commonly seen over the course
of the disease, where cardiac output returns to (or remains) normal, but SVR
becomes abnormally high. The chronic increase in cardiac afterload results in
concentric LVH and altered diastolic function. Hypertension also alters
cerebral autoregulation, such that normal cerebral blood flow is maintained in
the face of high blood pressures; autoregulation limits may be in the range of
mean blood pressures of 110–180 mm Hg.
The mechanisms responsible for the
changes observed in hypertensive patients seem to involve vascular hypertrophy,
hyperinsulinemia, abnormal increases in intracellular calcium, and increased
intracellular sodium concentrations in vascu-lar smooth muscle and renal
tubular cells. The increased intracellular calcium presumably results in
increased arteriolar tone, whereas the increased sodium concentration impairs
renal excretion of sodium. Sympathetic nervous system overactivity and enhanced
responses to sympathetic agonists are present in some patients. Hypertensive
patients sometimes display an exaggerated response to vasopressors and
vasodilators. Overactivity of the renin–angiotensin–aldosterone system seems to
play an important role in patients with accelerated hypertension.
Long-Term Treatment
Effective drug therapy reduces the
progression of hypertension and the incidence of stroke, conges-tive heart
failure, CAD, and renal damage. Effective treatment can also delay and
sometimes reverse con-comitant pathophysiological changes, such as LVH and
altered cerebral autoregulation.
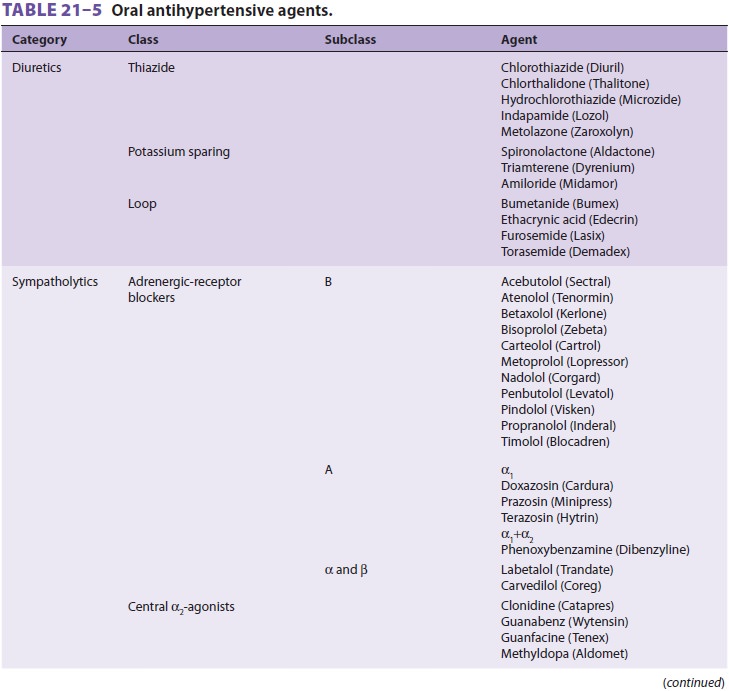
Some patients with mild hypertension
require only single-drug therapy, which may consist of a thi-azide diuretic,
ACE inhibitor, angiotensin-receptor blocker (ARB), β-adrenergic blocker, or calcium channel
blocker, although guidelines and outcome studies favor the first three options.
Concomitant illnesses should guide drug selection. All patients with a prior MI
should receive a β-adrenergic blocker and an ACE inhibitor (or ARB) to
improve outcomes, irrespective of the presence of hyperten-sion. In many
patients, the “guideline specified” agents will also be more than sufficient to
control hypertension.
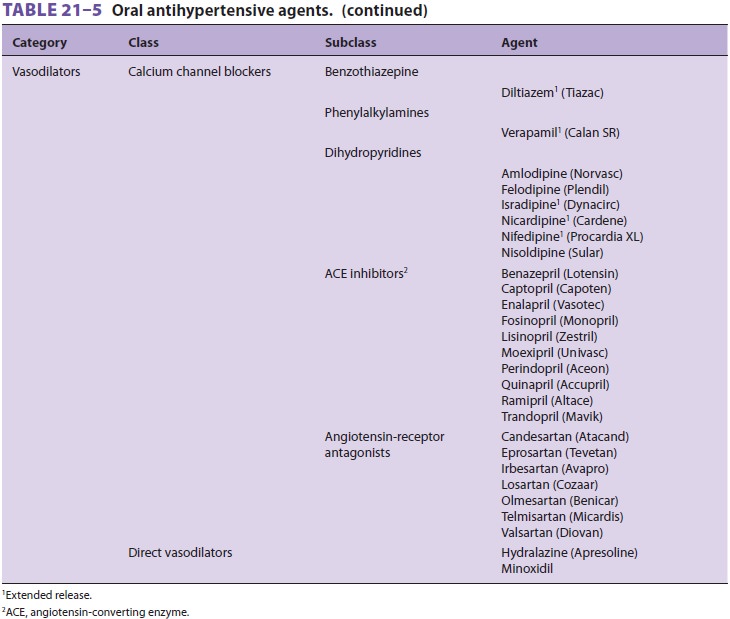
Patients with moderate to severe
hyperten-sion often require two or three drugs for control. The combination of
a diuretic with a β-adrenergic blocker and an ACE inhibitor is often
effective when single-drug therapy is not. As previously noted, ACE inhibitors
(or ARBs) prolong survival in patients with congestive heart failure, left
ventricular dys-function, or a prior MI. Familiarity with the names, mechanisms
of action, and side effects of commonly used antihypertensive agents is
important for anes-thesiologists (Table 21–5).
Related Topics