Chapter: Clinical Anesthesiology: Regional Anesthesia & Pain Management: Chronic Pain Management
Trigeminal Nerve Block
Somatic
Nerve Blocks
Trigeminal Nerve Block
A. Indications
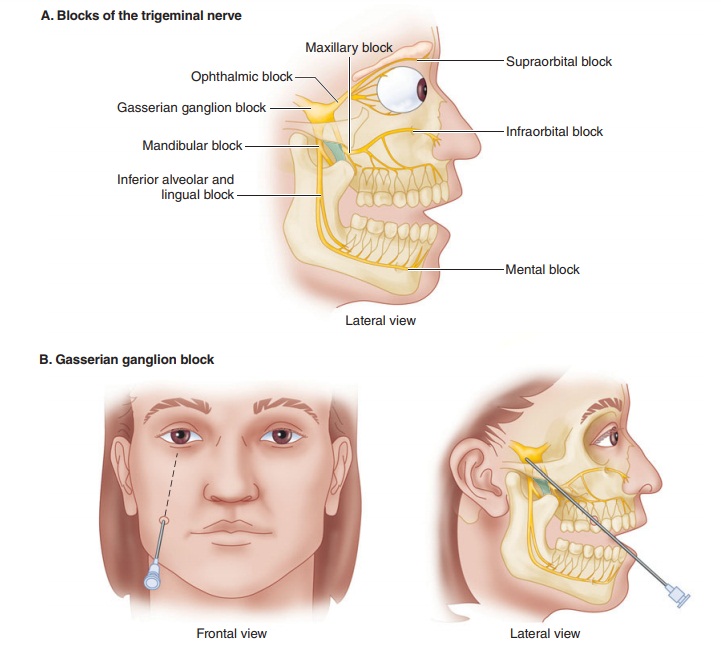
The two principal indications for trigeminal nerve block are trigeminal neuralgia and intractable facial cancer pain. Depending on the site of pain, these blocks may be performed on the gasserian ganglion itself, on one of the major divisions (ophthalmic, maxillary, or mandibular), or on one of their smaller branches.
B. Anatomy
The rootlets of cranial nerve V arise from the brain-stem and join one
another to form a crescent-shaped sensory (gasserian) ganglion in Meckel’s
cave. Most of the ganglion is invested with a dural sleeve. The three
subdivisions of the trigeminal nerve arise from the ganglia and exit the
cranium separately. (Figure 47–8A).
C. Technique
Gasserian
ganglion block—Fluoroscopic guid-ance is mandatory for the
performance of this pro-cedure ( Figure 47–8B).
An 8- to 10-cm 22-gauge needle is inserted approximately 3 cm lateral to the
angle of the mouth at the level of the upper second molar. The needle is then
advanced posteromedial-ly and angled superiorly to bring it into alignment with
the pupil in the anterior plane and with the mid-zygomatic arch in the lateral
plane. Without entering the mouth, the needle should pass be-tween the
mandibular ramus and the maxilla, and lateral to the pterygoid process to enter
the cra-nium through the foramen ovale. After a negative aspiration for
cerebrospinal fluid and blood, local anesthetic is injected.
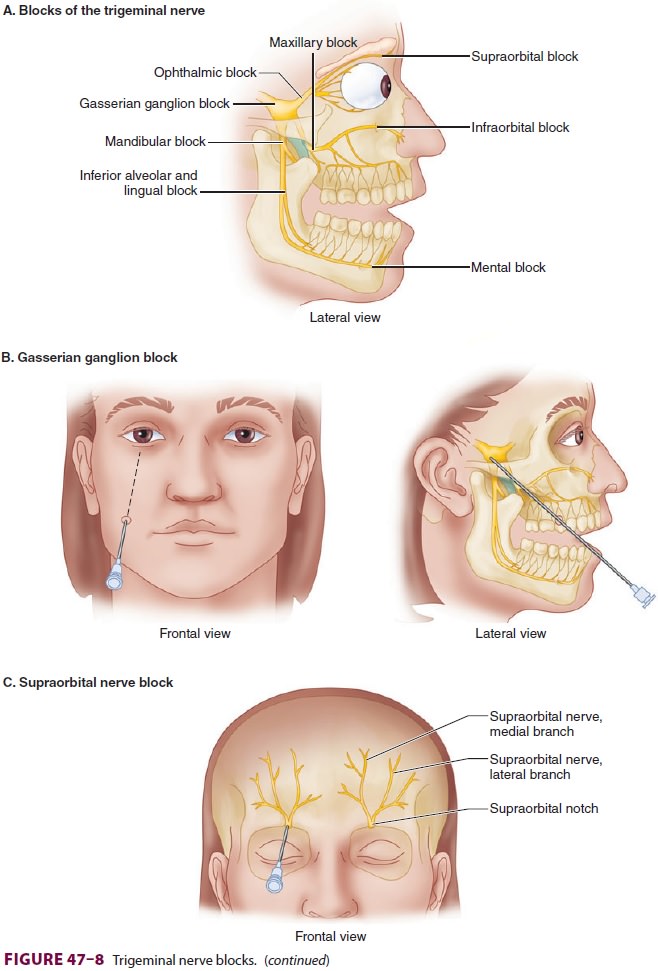
Blocks of the ophthalmic nerve and its
branches—In this procedure, to avoid denerva-tion-related keratitis, only the
supraorbital branch is blocked in most cases (Figure
47–8C); the oph-thalmic division itself is not blocked. The nerve is
easily located and blocked with local anesthetic at the supraorbital notch,
which is located on the su-praorbital ridge above the pupil. The supratrochlear
branch can also be blocked with local anesthetic at the superior medial corner
of the orbital ridge.
Blocks
of the maxillary nerve
and its branches—With the patient’s mouth
slightly opened, an 8- to 10-cm 22-gauge needle is inserted between the
zygomatic arch and the notch of the mandible (Figure 47–8D). After contact with the lateral pter-ygoid plate at about 4-cm depth
(position 1 in fig-ure), the needle is partially withdrawn and angled slightly
superiorly and anteriorly to pass into the
pterygopalatine fossa (position 2). Local anesthetic is injected once
paresthesias are elicited. Both the maxillary nerve and the sphenopalatine
(pterygo-palatine) ganglia are usually anesthetized by this technique. The
sphenopalatine ganglion (and ante-rior ethmoid nerves) can be anesthetized
transmu-cosally with topical anesthetic applied through the nose; several
cotton applicators soaked with local anesthetic (cocaine or lidocaine) are
inserted along the medial wall of the nasal cavity into the area of the
sphenopalatine recess. The sphenopalatine gan-glion blockade may be helpful for
patients with chronic nasal pain, cluster headache, or Sluder’s neuralgia.The
infraorbital branch of cranial nerve V passes through the infraorbital foramen,
where it can be blocked with local anesthetic. This foramen is approximately 1
cm below the orbit and is usu-ally located with a needle inserted about 2 cm
lateral to the nasal ala and directed superiorly, posteriorly, and slightly
laterally.
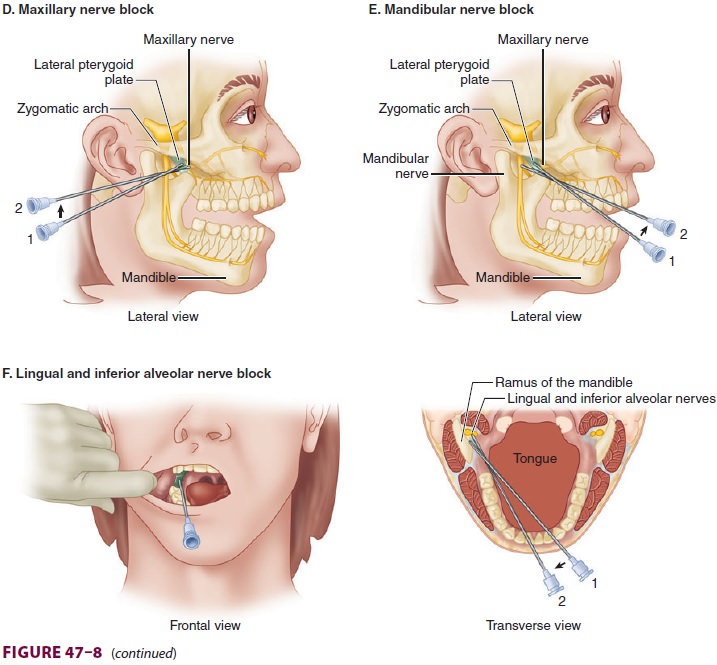
Blocks of the mandibular nerve and its
branches—With the patient’s mouth slightly opened (Figure 47–8E), an 8 to10-cm
22-gauge needle is inserted between the zygomatic arch and the man-dibular
notch. After contact with the lateral ptery-goid plate (position 1 in figure),
the needle is par-tially withdrawn and angled slightly superiorly and
posteriorly toward the ear (position 2). Local anes-thetic is injected once
paresthesias are elicited.
The lingual and inferior mandibular branches of the mandibular nerve may
be blocked intraorally utilizing a 10-cm 22-gauge needle ( Figure
47–8F). The patient is asked to open the mouth maximally and the coronoid
notch is palpated with the index finger of the nonoperative hand. The needle is
then introduced at the same level (approximately 1 cm above the surface of the
last molar), medial to the finger but lateral to the pterygomandibular plica
(position 1 in figure). It is advanced posteriorly 1.5–2 cm along the medial
side of the mandibular ramus, making contact with the bone (position 2). Both
nerves are usually blocked following injection of local anesthetic.
The terminal portion of the inferior alveolar nerve may be blocked as it
emerges from the mental foramen at the mid-mandible just beneath the cor-ner of
the mouth. Local anesthetic is injected once paresthesias are elicited or the
needle is felt to enter the foramen.
D. Complications
Complications of a gasserian ganglion block include accidental
intravascular injection, subarachnoid injection, Horner’s syndrome, and motor
block of the muscles of mastication. The potential for seri-ous hemorrhage is
greatest for blockade of the maxillary nerve. The facial nerve may be
uninten-tionally blocked during blocks of the mandibular division.
Related Topics