Chapter: Clinical Anesthesiology: Regional Anesthesia & Pain Management: Chronic Pain Management
Epidural Injections
Epidural
Injections
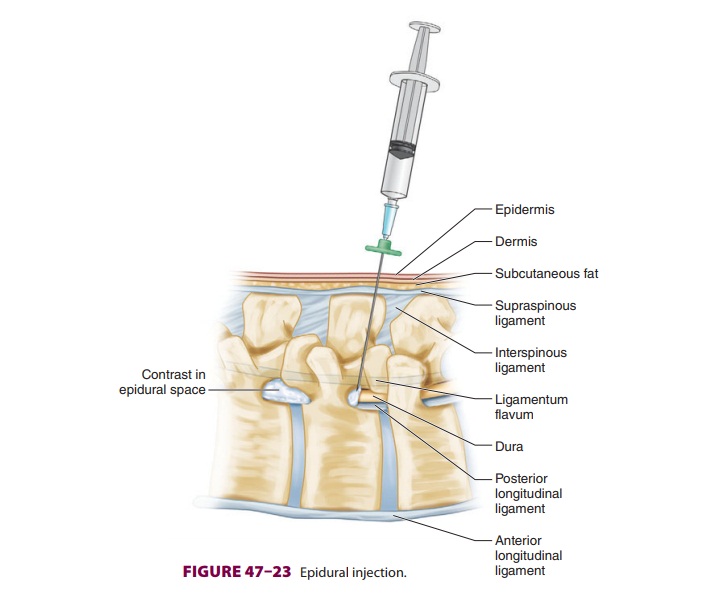
Epidural steroid injections ( Figure
47–23) are used for symptomatic relief of pain
associated with nerve root compression (radiculopathy). Pathological studies
often demonstrate inflammation following disc herniation. Clinical improvement
appears to be correlated with the resolution of nerve root edema. Epidural
steroid injections are clearly superior to local anesthetics alone. They are
most effective when given within 2 weeks of pain onset but appear to be of
little benefit in the absence of neural compres-sion or irritation. Long-term
studies have failed to show any persistent benefit after 3 months, and these
injections may change the time course of pain relief without changing long-term
outcomes.
The two most commonly used agents are meth-ylprednisolone
acetate (40–80 mg) and triamcino-lone diacetate (40–80 mg). Dexamethasone is
being used with increased frequency due to its smaller particulate size
(smaller than an erythrocyte). Intravascular injection of steroid suspension
with larger particulate size may lead to embolic compli-cations. The steroid
may be injected with diluent (saline) or local anesthetic in volumes of 6–10 mL
or 10–20 mL for lumbar and caudal injections, respec-tively. Simultaneous
injection of opioids offers no added benefit and may significantly increase
risks. The epidural needle should be cleared of the ste-roid prior to its
withdrawal to prevent formation of a fistula tract or skin discoloration.
Injection of local anesthetic along with the steroid can be help-ful if the
patient has significant muscle spasm, but it is associated with risks of
intrathecal, subdural, and intravascular injection. The presenting pain is
often transiently intensified following injection, and the local anesthetic
provides immediate pain relief until the steroidal antiinflammatory effects
take place, usually within 12–48 h.
Epidural steroid injections may be most
effec-tive when the injection is at the site of injury. Only a single injection
is given if complete pain relief is achieved. If there is a good but temporary
response, a second injection may be given 2–4 weeks later. Larger or more
frequent doses increase the risk of adrenal suppression and systemic side
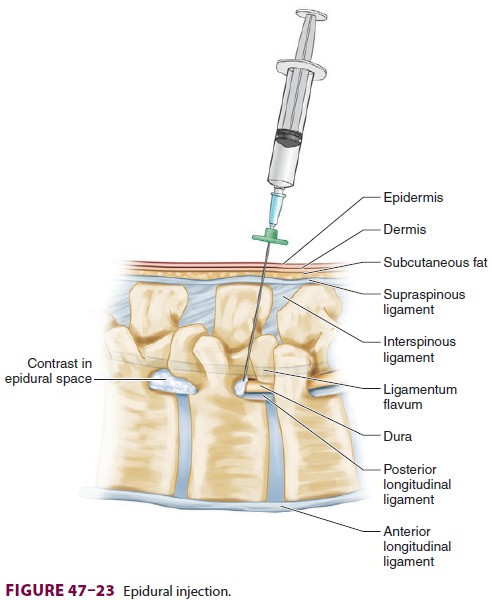
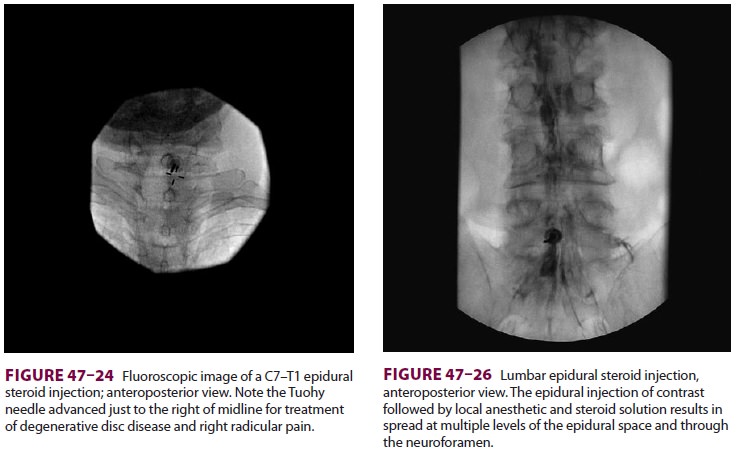
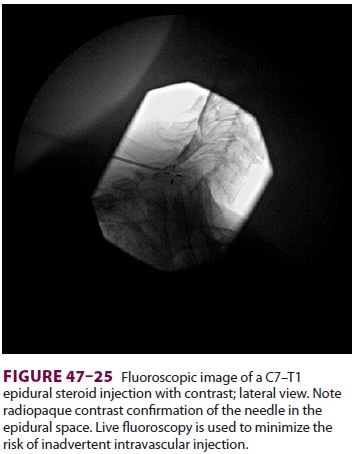
effects. Most pain practitioners utilize fluoroscopy for epidural injection and
confirm correct placement with injec-tion of radiopaque contrast ( Figures
47–24 through 47–26). A transforaminal epidural steroid injectionmay be more effective than
the standard interlami-nar epidural technique, especially for radicular pain.
The needle is directed under fluoroscopic guidance into the foramen of the
affected nerve root; contrast is then injected to confirm spread into the
epidural space and absence of intravascular injection prior to steroid
injection. This technique differs from a
selective nerve root block (SNRB) in two
important ways; with an SNRB, the needle does not enter the foramen and the
injected solution tracks along the nerve but not into the epidural space. The
SNRB may be helpful as a diagnostic procedure for the surgeon who is
considering a foraminotomy at a particular affected level based upon imaging,
clinical presenta-tion, and the results of the SNRB.
Caudal injection may be used in patients with
previous back surgery when scarring and anatomic distortion make lumbar
epidural injections more difficult. Unfortunately, migration of the steroid to
the site of injury may not be optimal. The use of a catheter to direct the
injection within the sacral and epidural canal may improve outcome.
However,above the level of S2, there is a risk of thecal perfora-tion with a
stylet-guided catheter. Intrathecal steroid injections are not recommended
because the ethyl-ene glycol preservative in the suspension has been implicated
in arachnoiditis following unintentional subarachnoid injections.
Related Topics