Chapter: Clinical Anesthesiology: Regional Anesthesia & Pain Management: Chronic Pain Management
Headache - Chronic Pain Management
HEADACHE
Headache is a common complaint that affects nearly everyone at some time
in life. In the vast majority of cases, headaches do not reflect a serious
underlying disorder and are not of sufficient sever-ity or frequency for the
individual to seek medi-cal attention. However, as with other complaints of
pain, the possibility of a clinically significant underlying disorder should
always be considered. The practitioner should solicit other associated symptoms
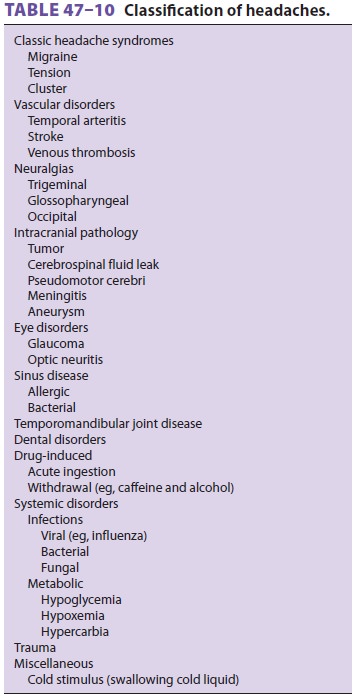
or clinical findings that suggest serious underlying pathology. Table
47–10 lists impor-tant causes of headache. Disorders in which the primary
complaint is headache are considered in the following discussion. As will
become apparent, there is significant variability in clinical presen-tation and
overlap in the symptoms of the major headache syndromes, particularly between
tension and migraine headaches.
Tension Headache
Tension headaches are classically described as tight bandlike pain or
discomfort that is often associated with tightness in the neck muscles. The
headache may be frontal, temporal, or occipital, more often bilateral than
unilateral. Intensity typically builds gradually and fluctuates, lasting hours
to days. They may be associated with emotional stress or depres-sion. Treatment
is symptomatic and consists of NSAIDs.
Migraine Headache
Migraine headaches are typically described as
throb-bing or pounding and are often associated with photophobia, scotoma,
nausea and vomiting, and localized transient neurological dysfunction (aura).
The latter may be sensory, motor, visual, or olfactory. Classic migraines by
definition are preceded by an aura, whereas common migraines are not. The pain
is usually unilateral but can be bilateral with a fron-totemporal location and
lasts 4–72 h. Migraines pri-marily affect children (both sexes equally) and
young adults (predominantly females). A family history is often present.
Provocation by odors, certain foods (eg, red wine), menses, and sleep
deprivation is com-mon. Sleep characteristically relieves the headache. The
mechanism is complex and may include vaso-motor, autonomic (serotonergic
brainstem systems), and trigeminal nucleus dysfunction. Treatment is both
abortive and prophylactic. Rapid abortive treatment includes oxygen,
sumatriptan (6 mg sub-cutaneously), dihydroergotamine (1 mg intramus-cularly or
subcutaneously), intravenous lidocaine (100 mg), nasal butorphanol (1–2 mg),
and sphe-nopalatine ganglion block. Other abortive options include zolmitriptan
nasal spray, dihydroergotaminenasal spray, or an oral serotonin 5-HT 1B/1D-receptor agonist (almotriptan, frovatriptan,
naratriptan, rizatriptan, eletriptan, or sumatriptan). Prophylactic treatment
may include β-adrenergic blockers,
cal-cium channel blockers, valproic acid, amitriptyline, and onabotulinumtoxinA
(Botox) injections.
Cluster Headache
Cluster headaches are classically unilateral
and periorbital, occurring in clusters of one to three attacks a day over a 4-
to 8-week period. The pain is described as a burning or drilling sensation that
may awaken the patient from sleep. Each episode lasts 30–120 min. Remissions
lasting a year at a time are common. Red eye, tearing, nasal stuffiness,
pto-sis, and Horner’s syndrome are classic findings. The headaches are
typically episodic but can become chronic without remissions. Cluster headaches
primarily affect males (90%). Abortive treatments includes oxygen and
sphenopalatine block. Lithium, a short course of steroid medication, and
verapamil may be used for prophylaxis.
Temporal Arteritis
Temporal arteritis is an inflammatory
disorder of extracranial arteries. The headache can be bilateral or unilateral
and is located in the temporal area in at least 50% of patients. The pain
develops over a few hours, is usually dull in quality but may be lancinating at
times and worse at night and in cold weather. Scalp tenderness is usually
present. Temporal arteritis is often accompanied by polymyalgia rheumatica,
fever, and weight loss. It is a relatively common disorder of older patients (>55 years), with an incidence of about 1 in
10,000 per year and a slight female predomi-nance. Early diagnosis and
treatment with steroids is important because progression can lead to blindness
through involvement of the ophthalmic artery.
Trigeminal Neuralgia
Trigeminal neuralgia (or tic douloureux) is classically unilateral and usually located inthe
V2 or V3 distribution of the trigeminal nerve. It has an electric shock quality
lasting from seconds to minutes at a time and is often provoked by contact with
a discrete trigger. Facial muscle spasm may be present. Patients are
middle-aged and elderly, with a 2:1 female to male ratio. Common causes of
tri-geminal neuralgia include compression of the nerve by the superior
cerebellar artery as it exits the brain-stem, cerebellopontine angle tumor, or
multiple sclerosis. The drug of choice for treatment is carbam-azepine although
it carries a risk of agranulocytosis. Phenytoin or baclofen may be added,
particularly if patients do not tolerate the required doses of car-bamazepine.
More invasive treatments for patients who do not respond to drug therapy
include glycerol injection, radiofrequency ablation, balloon com-pression of
the gasserian ganglion, and microvascu-lar decompression of the trigeminal
nerve.
Related Topics