Chapter: Clinical Anesthesiology: Regional Anesthesia & Pain Management: Chronic Pain Management
Evaluation of the Patient with Chronic Pain
Evaluation of the Patient with Chronic Pain
The evaluation of any patient with pain
should include several key components. Informationabout location, onset, and
quality of pain, as well as alleviating and exacerbating factors, should be
obtained, along with a pain history that includes pre-vious therapies and
changes in symptoms over time. In addition to physical symptoms, chronic pain
usu-ally involves a psychological component that should be addressed as well.
Questionnaires, diagrams, and pain scales are useful tools in helping patients
ade-quately describe the characteristics of their pain and how it affects their
quality of life. Information gath-ered during the physical examination can help
dis-tinguish pain location, type, and systemic sequelae, if any. Imaging
studies such as plain radiographs, computed tomography (CT), magnetic resonance
imaging (MRI), and bone scans can often suggest physiological causes. All
components are necessary for a comprehensive evaluation of the pain patient prior
to determining appropriate treatment options.
PAIN MEASUREMENT
Reliable quantitation of pain severity helps deter-mine therapeutic
interventions and evaluate the efficacy of treatments. This is a challenge,
however, because pain is a subjective experience that is influ-enced by
psychological, cultural, and other variables. Clear definitions are necessary,
because pain may be described in terms of tissue destruction or bodily or
emotional reaction.
The numerical rating scale, Wong-Baker FACES rating scale, visual analog
scale (VAS), and McGill Pain Questionnaire (MPQ) are most commonly used. In the
numerical scale, 0 corresponds to no pain and 10 is intended to reflect the worst possible pain. The Wong-Baker FACES pain scale, designed for
children 3 years of age and older, is useful in patients with whom
communication may be difficult. The patient is asked to point to various facial
expressions rang-ing from a smiling face (no pain) to an extremely unhappy one
that expresses the worst possible pain. The VAS is a 10-cm horizontal line
labeled “no pain” at one end and “worst pain imaginable” on the other end. The
patient is asked to mark on this line where the intensity of the pain lies. The
distance from “no pain” to the patient’s mark numerically quantifies the pain.
The VAS is a simple and efficient method that correlates well with other
reliable methods.
The MPQ is a checklist of words describ-ing symptoms. Unlike other pain
rating methods that assume pain is one-dimensional and describe intensity but
not quality, the MPQ attempts to define the pain in three major dimensions:
(1) sensory–discriminative
(nociceptive pathways), (2) motivational–affective (reticular and limbic
structures), and (3) cognitive–evaluative (cerebral cortex). It contains 20
sets of descriptive words that are divided into four major groups: 10 sensory,
5 affective, 1 evaluative, and 4 miscellaneous. The patient selects the sets
that apply to his or her pain and circles the words in each set that best
describe the pain. The words in each class are given rank according to severity
of pain. A pain rating index is derived based on the words chosen.
PSYCHOLOGICAL EVALUATION
Psychological evaluation is useful whenever
medical evaluation fails to reveal an apparentcause for pain, when pain
intensity, characteristics, or duration are disproportionate to disease or
injury, or when depression or other psychological issues are apparent. These
types of evaluations help define the role of psychological or behavioral
factors. The most commonly used tests are the Minnesota Multiphasic Personality
Inventory (MMPI) and Beck Depression Inventory.
The MMPI is a 566-item true–false
question-naire that attempts to define the patient’s personality on 10 clinical
scales. Three validity scales serve to identify patients deliberately trying to
hide traits or alter the results. Cultural differences can affect
scores.Moreover, the test is lengthy and some patients find its questions
insulting. The MMPI is used primar-ily to confirm clinical impressions about the
role of psychological factors; it cannot reliably distinguish between “organic”
and “functional” pain.
Depression is very common in patients with chronic pain. It is often
difficult to determine the relative contribution of depression to the suffering
associated with pain. The Beck Depression Inven-tory is a useful test for
identifying patients with major depression.
Several tests have been developed to assess functional limitations or
impairment (disability). These include the Multidimensional Pain Inventory
(MPI), Medical Outcomes Survey 36-Item Short Form (SF-36), Pain Disability
Index (PDI), and Oswestry Disability Index (ODI).
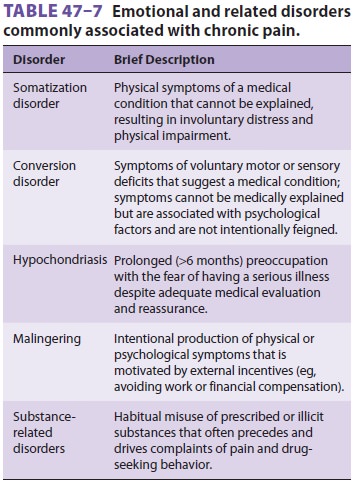
Emotional disorders are commonly associated
with complaints of chronic pain, and chronic pain often results in varying degrees
of psychological dis-tress. Determination of which came first is often
dif-ficult. In either case, both the pain and emotional distress need to be
treated. Table 47–7 lists emo-tional
disorders in which treatment should be pri-marily directed at the emotional
disorder.
ELECTROMYOGRAPHY & NERVE CONDUCTION STUDIES
Electromyography and nerve conduction studies complement one another and
are useful for con-firming the diagnosis of entrapment syndromes, radicular
syndromes, neural trauma, and poly-neuropathies. They can often distinguish
between neurogenic and myogenic disorders. Patterns of abnormalities can
localize a lesion to the spinal cord, nerve root, limb plexus, or peripheral
nerve. In addi-tion, they may also be useful in excluding “organic” disorders
when psychogenic pain or a “functional” syndrome is suspected.
Electromyography employs needle electrodes to record potentials in individual muscles. Mus-cle potentials are recorded first while the muscle is at rest and then as the patient is asked to move the muscle. A triphasic motor unit action poten-tial is normally seen as the patient voluntarily moves the muscle. Abnormal findings suggestive of denervation include persistent insertion poten-tials, the presence of positive sharp waves, fibrillary activity, or fasciculation potentials. Abnormalities in muscles produce changes in amplitude and duration as well as polyphasic action potentials.
Peripheral nerve conduction studies employ supramaximal stimulations of
motor or mixed sen-sorimotor nerve, whereas muscle potentials are recorded over
the appropriate muscle. The time between the onset of the stimulation and the
onset of the muscle potential (latency) is a measurement of the fastest
conducting motor fibers in the nerve. The amplitude of the recorded potential
indicates the number of functional motor units, whereas its duration reflects
the range of conduction velocities in the nerve. Conduction velocity can be
obtained by stimulating the nerve from two points and com-paring the latencies.
When a pure sensory nerve is evaluated, the nerve is stimulated while action
potentials are recorded either proximally or distally (antidromic
conduction).Nerve conduction studies distinguish between mononeuropathies (due
to trauma, compression, or entrapment) and polyneuropathies. The latter include
systemic disorders that may produce abnor-malities that are widespread and
symmetrical or that are random (eg, mononeuropathy multiplex).
Related Topics