Chapter: Clinical Anesthesiology: Regional Anesthesia & Pain Management: Chronic Pain Management
Cervical Paravertebral Nerve Blocks
Cervical Paravertebral Nerve Blocks
A. Indications
Cervical paravertebral nerve blocks can be useful diagnostically and
therapeutically for patients with cervical disc displacement, cervical
foraminal steno-sis, or cancer-related pain originating from the cer-vical
spine or shoulder.
B. Anatomy
The cervical spinal nerves lie in the sulcus of the transverse process
of their respective vertebral lev-els. As noted earlier, unlike thoracic and
lumbar nerve roots, those in the cervical spine exit the foramina above the vertebral bodies for which
they are named.
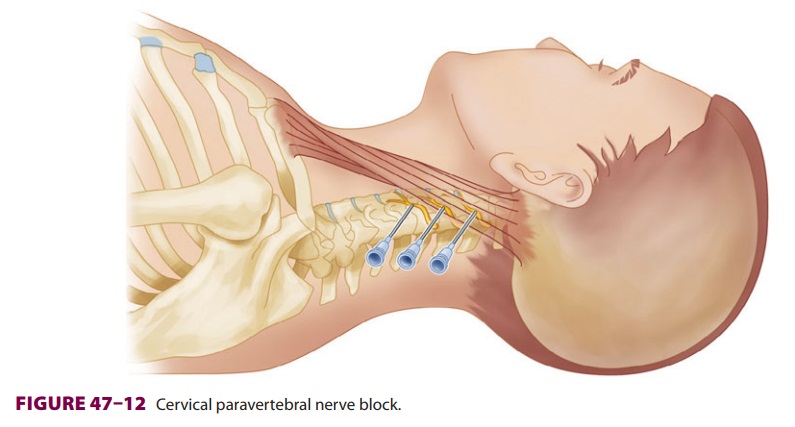
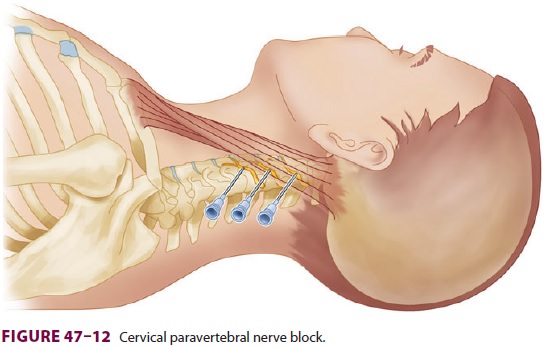
C. Technique
The lateral approach is most commonly used to block C2–C7 (Figure
47–12). Patients are asked to turn
the head to the opposite side while in a sitting or supine position. A line is
then drawn between the mastoid process and Chassaignac’s tubercle (the tubercle
of the C6 transverse process). A series of injections are made with a 5-cm
22-gauge needle along a second parallel line 0.5 cm posterior to the first
line. In the case of diagnostic blocks, a smaller injectate volume may be
helpful in order to minimize local anesthetic spread to adjacent structures and
thereby increase block specificity. Because the transverse process of C2 is
usually difficult to palpate, the injection for this level is placed 1.5 cm
beneath the mastoid process. The other transverse processes are usually
inter-spaced 1.5 cm apart and are 2.5–3 cm deep. Fluoros-copy is useful in
identifying specific vertebral levels during diagnostic blocks. This procedure
may also be performed with ultrasound guidance.
D. Complications
Unintentional intrathecal or epidural anesthe-sia at this level rapidly causes respiratory paralysis and hypotension. Injection of even small volumes of local anesthetic into the vertebral artery causes unconsciousness and seizures. Other complications include Horner’s syndrome, as well as blockade of the recurrent laryngeal and phrenic nerves.
Embolic cerebrovascular and spinal cord com-plications have resulted
from injection of particulate steroid with this block. Particulate steroid
should not be used with cervical paravertebral nerve blocks because of possible
anomalous vertebral artery anat-omy in this region.
Related Topics