Chapter: Clinical Anesthesiology: Regional Anesthesia & Pain Management: Chronic Pain Management
Low Back Pain & Related Syndromes
LOW BACK PAIN & RELATED SYNDROMES
Back pain is an extremely common complaint
and a major cause of work disability worldwide. Lum-bosacral strain,
degenerative disc disease, and myo-fascial syndromes are the most common
causes. Low back pain, with or without associated leg pain, may also have
congenital, traumatic, degenerative, inflammatory, infectious, metabolic,
psychologi-cal, and neoplastic causes. Moreover, back pain can be due to
disease processes in the abdomen andpelvis, particularly those affecting
retroperitoneal structures (pancreas, kidneys, ureters, and aorta), the uterus
and adnexa, the prostate, and the recto-sigmoid colon. Disorders of the hip can
also mimic back disorders. A positive Patrick’s sign (or Patrick’s test)—ie,
the elicitation of pain in the hip or sacro-iliac joint when the examiner
places the ipsilateral heel of the supine patient on the contralateral knee and
presses down on the ipsilateral knee—helps identify back pain due to hip or
sacroiliac joint dis-orders. This sign is also referred to by an acronym, FABERE
(sign), because the movement of the leg involves flexion, abduction, external rotation, and extension.
1. Applied Anatomy of the Back
The back can be described in terms of anterior and posterior elements. The anterior elements consist ofcylindrical vertebral
bodies interconnected by inter-vertebral discs and supported by anterior and
poste-rior longitudinal ligaments. The posterior elements are bony arches
extending from each vertebral body, consisting of two pedicles, two transverse
processes, two laminae, and a spinous process. The transverse and spinous
processes provide points of attachment for the muscles that move and protect
the spinal col-umn. Adjacent vertebrae also articulate posteriorly by two
gliding facet joints.
Spinal structures are innervated by the sinu-vertebral branches and
posterior rami of spinal nerves. The sinuvertebral nerve arises before each
spinal nerve divides into anterior and posterior rami, and reenters the
intervertebral foramen to innervate the posterior longitudinal ligament, the
posterior annulus fibrosus, periosteum, dura, and epidural vessels. Paraspinal
structures are supplied by the posterior primary ramus. Each facet joint is
innervated by the medial branch of the posterior primary rami of the spinal
nerves above and below the joint.
As lumbar spinal nerve roots exit the dural
sac, they travel down 1–2 cm laterally before exit-ing through their respective
intervertebral foramina; thus, for example, the L5 nerve root leaves the dural
sac at the level of the L4–L5 disc (where it is more likely to be compressed)
but leaves the spinal canal beneath the L5 pedicle opposite the L5–S1 disc.
2.Paravertebral Muscle & Lumbosacral Joint Sprain/Strain
Approximately 80–90% of low back pain is due
to sprain or strain associated with lifting heavy objects, falls, or sudden
abnormal movements of the spine. The term sprain
is generally used when the pain is related to a well-defined acute injury,
whereas strain is used when the pain
is more chronic and is likely related to repetitive minor injuries.
Injury to paravertebral muscles and ligaments
results in reflex muscle spasm, which may or may not be associated with trigger
points. The pain is usually dull and aching, and occasionally radiates down the
buttocks or hips. Sprain is a self-limited benign pro-cess that resolves in 1–2
weeks. Symptomatic treat-ment consists of rest and oral analgesics.
The sacroiliac joint is particularly vulnerable to rotational injuries.
It is one of the largest joints in the body and functions to transfer weight
from the upper body to the lower extremities. Acute or chronic injury can cause
slippage, or subluxation, of the joint. Pain originating from this joint is
char-acteristically located along the posterior ilium and radiates down the
hips and posterior thigh to the knees. The diagnosis is suggested by tenderness
on palpation, particularly on the medial aspect of the posterior superior iliac
spine, and by compression of the joints. Pain relief following injection of the
joint with local anesthetic (3 mL) is diagnostic and may also be therapeutic.
Injection of intraarticular steroid medication may be considered. For
poten-tially longer duration of analgesia, radiofrequency ablation may be
performed at the dorsal ramus of L5 as well as the lateral branches of the S1,
S2, and S3 nerves if the patient responded well to local anes-thetic injections
of the sacroiliac joint or to diagnos-tic injections of these nerves.
3. Buttock Pain
Buttock pain may be due to several different fac-tors, and can be quite
debilitating. Coccydynia (or, coccygodynia) may the result of trauma to the
coc-cyx or surrounding ligaments. It may resolve by means of physical therapy,
coccygeal nerve blocks to the lateral aspects of the coccyx, or ablative or
neuromodulatory techniques. Piriformis syndromepresents as pain in the buttock,
which can be accom-panied by numbness and tingling in distribution of the
sciatic nerve. The nerve may or may not be entrapped. Injection of local
anesthetic into the belly of this muscle or into trigger points located at the
origin and insertion of the muscle may help relieve the pain.
4. Degenerative Disc Disease
Intervertebral discs bear at least one third of the weight of the spinal
column. Their central portion, the nucleus pulposus, is composed of gelatinous
material early in life. This material degenerates and becomes fibrotic with
advancing age and follow-ing trauma. The nucleus pulposus is ringed by the
annulus fibrosus, which is thinnest posteriorly and bounded superiorly and
inferiorly by cartilaginous plates. Disc (discogenic) pain may be due to one of
two major mechanisms: (1) protrusion or extru-sion of the nucleus pulposus
posteriorly or (2) loss of disc height, resulting in the reactive formation of
bony spurs (osteophytes) from the rims of the ver-tebral bodies above and below
the disc. Degenera-tive disc disease most commonly affects the lumbar spine
because it is subjected to the greatest motion and because the posterior
longitudinal ligament is thinnest at L2–L5. Factors such as increased body
weight and cigarette smoking may play a role in the development of lumbar disc
disease. The role of the disc in producing chronic back pain is not clearly
understood. In patients with persistent axial low back pain, the history and
physical examination may provide clues. If the patient has pain when sitting or
standing, or maintaining a certain position for an extended period of time,
there may be an element of discogenic pain.
Discography is a procedure that is often used
to try to provide some objective evidence of the role of a given disc in
producing a patient’s back pain. After a needle is inserted into the disc, the
opening pressure can be assessed; a subsequent injection of radiocontrast
material produces increased pressure that may reproduce the patient’s pain and
may pro-vide radiographic identification of anatomic abnor-malities within the
disc (eg, a rent or tear). It the pain produced with injection is similar to
that which the patient experiences on a daily basis, it is deemed concordant pain. If
not, it is deemed discordant. Insome
circumstances, the pressure in the disc fol-lowing injection is not
significantly higher than the opening pressure. This may be due to the presence
of a fissure in the disc that tracks to the epidural space. Risks of
discography include infection and discitis, which may be difficult to treat
because the disc is relatively avascular.
Treatment options for discogenic pain include conservative therapy,
steroid injections into the disc, intradiscal biacplasty, involving heating the
poste-rior annulus of the disc by way of radiofrequency ablation, and surgical
fusion with bone graft or hardware placement; each has shown mixed degrees of
success. The evaluation and treatment of disco-genic pain is an area of significant
controversy and ongoing research.
Herniated (Prolapsed) Intervertebral Disc
Weakness and degeneration of the annulus
fibrosus and posterior longitudinal ligament can cause her-niation of the
nucleus pulposus posteriorly into the spinal canal. Ninety percent of disc
hernia-tions occur at L5–S1 or L4–L5. Symptoms usually develop following
flexion injuries or heavy lifting and may be associated with bulging,
protru-sion, or extrusion of the disc. Disc herniations usu-ally occur
posterolaterally and often result in compression of adjacent nerve roots,
producing pain that radiates along that dermatome (radiculopathy). Sciatica describes pain along the
sciatic nerve due tocompression of the lower lumbar nerve roots. When disc
material is extruded through the annulus fibro-sus and posterior longitudinal
ligament, free frag-ments can become wedged in the spinal canal or the
intervertebral foramina. Less commonly a large disc bulges or large fragments
extrude posteriorly, compressing the cauda equina in the dural sac; in these
instances patients can experience bilateral pain, urinary retention, or, less
commonly, fecal incontinence.
Pain associated with disc disease is
aggravated by bending, lifting, prolonged sitting, or anything that increases
intraabdominal pressure, such as sneezing, coughing, or straining. It is
usually relieved by lying down. Numbness or weakness is indicative
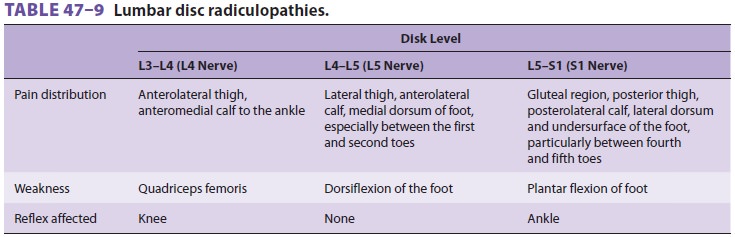
of radiculopathy (Table 47–9). Bulging of the disc through
the posterior longitudinal ligament can also produce low back pain that
radiates to the hips or buttocks. Straight leg-raising tests may be used to
assess nerve root compression. With the patient supine and the knee fully
extended, the leg on the affected side is raised and the angle at which the
pain develops is noted; dorsiflexion of the ankle with the leg raised typically
exacerbates the pain by further stretching the lumbosacral plexus. Pain while
raising the contralateral leg is an even more reliable sign of nerve
compression.
The use of MRI has increased dramatically in
the past decade in association with a two- to three-fold increase in back
surgeries, although this has not correlated with improved patient outcome. The
American Pain Society’s clinical practice guidelines for low back pain do not
recommend routine imag-ing or other diagnostic tests for patients with
nonspe-cific low back pain. Up to 30–40% of asymptomatic persons have
abnormalities of spinal structures on CT or MRI. In addition, the patient’s
awareness of his or her imaging abnormalities may influence self-perception of
health and functional ability.
Imaging studies and further tests should be
acquired when severe or progressive neurological deficits are present, or when
serious underlying con-ditions are suspected. CT myelography is the most
sensitive test for evaluating subtle neural compres-sion. Discography may be
considered when the pain pattern does not match the clinical findings. A
centrally herniated disc will usually cause pain at the lower level, and a
laterally protruded disc will cause pain at the same level as the disc. For
example, a centrally located disc herniation at L4–L5 may compress the L5 nerve
root whereas a laterally located disc herniation at this level may compress the
L4 nerve root.
The natural course of herniated disc
disor-ders is generally benign and the duration of pain is usually less than 2
months. Over 75% of patients treated nonsurgically, even those with
radiculopa-thy, have complete or near-complete pain relief. The goals of
treatment should therefore be to allevi-ate the pain and rehabilitate the
patient to return to a functional quality of life. Acute back pain due to a
herniated disc can be initially managed with modification of activity and with
medications such as NSAIDs and acetaminophen. A short course of opioids may be
considered for patients with severe pain. After the acute symptoms subside, the
patient can be referred to a physical therapist for instruc-tion on exercises
to improve lower back health. Patients who smoke tobacco should be advised to
stop smoking, not only for the obvious health ben-efits but also because
nicotine further compromises blood flow to the relatively avascular
intervertebral disc. Percutaneous disc decompression involving extraction of a
small amount of nucleus pulposus may help to decompress the nerve root. For
patients with acute-onset weakness correlating with the level of the disc
herniation, surgical management should be considered.
When symptoms persist beyond 3 months,
the pain may be considered chronic and may require a multidisciplinary
approach. Physical therapy continues to be a very important component of
rehabilitation. NSAIDs and antidepressants are also helpful, and percutaneous
interventions may be con-sidered. Of note, back supports should be discour-aged
because they may weaken paraspinal muscles.
Spinal Stenosis
Spinal stenosis is a disease of advancing
age. Degen-eration of the nucleus pulposus reduces disc height and leads to
osteophyte formation (spondylosis) at the endplates of adjoining vertebral
bodies. In con-junction with facet joint hypertrophy and with liga-mentum
flavum hypertrophy and calcification, this process leads to progressive
narrowing of the neural foramina and spinal canal. Neural compression may cause
radiculopathy that mimics a herniated disc. Extensive osteophyte formation may
compress multiple nerve roots and cause bilateral pain. The back pain usually
radiates into the buttocks,thighs, and legs. It is characteristically worse
with exercise and relieved by rest, particularly sitting with the spine flexed
(the “shopping cart sign”). The terms pseudoclaudication
and neurogenic claudication areused
to describe such pain that develops with pro-longed standing or ambulation. The
diagnosis is sug-gested by the clinical presentation and is confirmed by MRI,
CT, or myelography. Electromyography and nerve conduction studies may be useful
in evaluat-ing neurological compromise.
Patients with mild to moderate stenosis and
radicular symptoms may obtain benefit from epi-dural steroid injections via a
transforaminal, inter-laminar, or caudal approach. This may help these
individuals tolerate physical therapy. Those with moderate to severe stenosis
may be amenable to more recently developed procedures, such as the minimally
invasive lumbar decompression (MILD) procedure, which involves percutaneously
sculpting the lamina and ligamentum flavum to reduce central canal compression.
Severe multilevel symptoms may warrant surgical decompression.
5. Facet Syndrome
Degenerative changes in the facet
(zygapophyseal) joints may also produce back pain. Pain may be near the
midline; may radiate to the gluteal region, thigh,and knee; and may be
associated with muscle spasm. Hyperextension and lateral rotation of the spine
usually exacerbate the pain. The diagnosis may be confirmed if pain relief is
obtained following intraar-ticular injection of local anesthetic solution into
affected joints or by blockade of the medial branch of the posterior division
(ramus) of the spinal nerves that innervate them. Long-term studies suggest
that medial branch nerve blocks are more effective than facet joint injections.
Medial branch rhizotomy may provide long-term analgesia for patients with facet
joint disease.
6. Cervical Pain
Although most spine-related pain due to disc
dis-ease, spinal stenosis, or degenerative changes in the zygapophyseal joints
is felt in the low back and lower extremities, patients may have cervical pain
attrib-uted to these processes. A key anatomic difference is that the cervical
nerve roots, unlike those in the thoracic and lumbar spine, exit the foramina
above the vertebral bodies for which they are named. This occurs until the
level of C7, where the extra cervi-cal nerve roots, C8, exit below the pedicles
of C7, thus transitioning to the nomenclature of the tho-racic- and
lumbar-level vertebral bodies and nerve root denominations. The clinical
examination may help to identify the nerve root that is affected with
confirmation by a selective nerve root block. Risks inherent with percutaneous
cervical procedures include accidental intravascular injection of local
anesthetic or steroid. Particulate steroid injections in the neck have been
associated with devastating outcomes such as spinal cord injury and death and
should be avoided.
For primarily axial pain in the neck with extension into the head or to
the shoulders, cervi-cal medial branch blocks may clarify the diagnosis.
Long-term analgesia may be obtained with radiofre-quency ablation of the medial
branches innervating the zygapophyseal joints.
7. Congenital Abnormalities
Congenital abnormalities of the back are often asymptomatic and remain
occult for many years. Abnormal spinal mechanics can
make the patient prone to back pain, and in some instances, pro-gressive
deformities. Relatively common anomalies include sacralization of L5 (the
vertebral body is fused to the sacrum), lumbarization of S1 (it func-tions as a
sixth lumbar vertebra), spondylolysis (a disruption of the pars
interarticularis), spondylolis-thesis (displacement anteriorly of one vertebral
body on the next due to disruption of the posterior ele-ments, usually the
pars), and spondyloptosis (sub-luxation of one vertebral body on another
resulting in one body in front of the next). The diagnosis is made
radiographically. Spinal fusion may be nec-essary in patients with progressive
symptoms and spinal instability.
8. Tumors
Benign primary tumors of the spine include hem-angiomas, osteomas,
aneurysmal bone cysts, and eosinophilic granulomas. Malignant spine tumors
include osteosarcomas, Ewing’s sarcoma, and giant cell tumors. In addition,
breast, lung, prostate, renal, gastrointestinal, and thyroid carcinomas,
lympho-mas, and multiple myelomas frequently metasta-size to the lumbar spine.
Pain is usually constant and may be associated with localized tenderness over
involved vertebrae. Bony destruction, with or without neural or vascular
compression, produces the pain. Intradural tumors such as meningiomas,
schwannomas, ependymomas, and gliomas can present with a radiculopathy and may
rapidly prog-ress to flaccid paralysis. The primary site may be asymptomatic or
difficult to localize, thus requiring imaging studies for diagnosis. Treatment
options usually involve surgical decompression, chemo-therapy, radiation
therapy, and palliative symptom relief.
9. Infection
Bacterial infections of the spine usually
begin as dis-citis before progressing to osteomyelitis, and can be due to
pyogenic as well as tuberculous organisms. Patients may present with chronic
back pain with-out fever or leukocytosis (eg, spinal tuberculosis). Those with
acute discitis, osteomyelitis, or epidural abscess present with acute pain,
fever, leukocytosis, elevated sedimentation rate, and elevated C-reactive
protein, warranting immediate initiation of antibiot-ics. Urgent surgical
intervention is indicated when the patient also suffers from acute weakness.
10. Arthritides
Ankylosing spondylitis is a familial disorder
that is associated with histocompatibility antigen HLA-B27. It typically
presents as low back pain associated with early morning stiffness in a young
patient, usu-ally male. The pain has an insidious onset and may initially
improve with activity. After a few months to years, the pain gradually
intensifies and is associated with progressively restricted movement of the
spine. Diagnosis may be difficult early in the disease, but radiographic
evidence of sacroiliitis is usually pres-ent. As the disease progresses, the
spine develops a characteristic “bamboo-like” radiographic appear-ance. Some
patients develop arthritis of the hips and shoulders, as well as extraarticular
inflamma-tory manifestations. Treatment is primarily directed at functional
preservation of posture. NSAIDs, particularly indomethacin, are effective
analge-sics that reduce the early morning stiffness. Anti– tumor necrosis
factor-α agents have been shown
to decrease the progression of ankylosing spondylitis when administered early
in the course of therapy. These agents include infliximab (Remicaid),
etan-ercept (Enbrel), adalimumab (Humira), and golim-umab (Simponi). Although
this treatment approach shows promise, patients may be at an increased risk for
infection and the development of lymphoma.
Patients with Reiter’s syndrome, psoriatic arthritis, or inflammatory
bowel disease may also present with low back pain, but extraspinal
mani-festations are usually more prominent. Rheumatoid arthritis usually spares
the spine except for the zyg-apophyseal joints of the cervical spine.
Related Topics