Chapter: Clinical Anesthesiology: Regional Anesthesia & Pain Management: Chronic Pain Management
Definitions & Classification of Chronic Pain
DEFINITIONS & CLASSIFICATION OF PAIN
Like other conscious sensations, normal pain
per-ception depends on specialized neurons that func-tion as receptors,
detecting the stimulus, and then transducing and conducting it to the central
nervous system. Sensation is often described as either proto-pathic (noxious)
or epicritic (nonnoxious). Epicritic sensations (light touch, pressure,
proprioception, and temperature discrimination) are characterized by
low-threshold receptors and are generally con-ducted by large myelinated nerve
fibers. In con-trast, protopathic sensations (pain) are detected by
high-threshold receptors and conducted by smaller, lightly myelinated (Aδ) and unmyelinated (C) nerve fibers.
What Is Pain?
Pain is not just a sensory modality but an experi-ence. The
International Association for the Study of Pain defines pain as “an unpleasant
sensory and emotional experience associated with actual or potential tissue
damage, or described in terms of such damage.” This definition recognizes the
inter-play between the objective, physiological sensory aspects of pain and its
subjective, emotional, and psychological components. The response to pain can
be highly variable among different individuals as well as in the same person at
different times.
The term nociception is
derived from noci (Latin for harm or
injury) and is used to describe neural responses to traumatic or noxious
stimuli. All nociception produces pain, but not all pain results from
nociception. Many patients experience pain in the absence of noxious stimuli.
It is there-fore clinically useful to divide pain into one of two
categories: (1) acute pain, which is
primarily due to nociception, and (2) chronic pain, which may be due to
nociception, but in which psychological and behavioral factors often play a
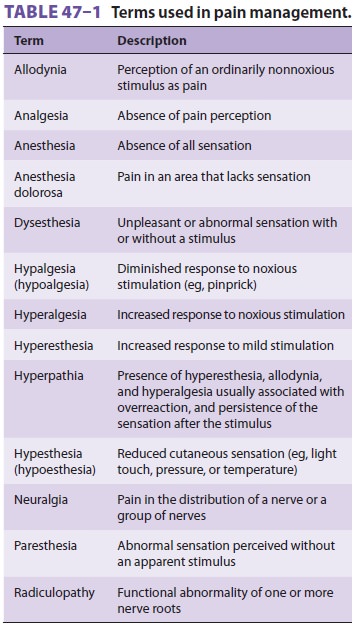
major role. Table 47–1 lists terms frequently
used in describing pain.Pain may also be classified according to
patho-physiology (eg, nociceptive or neuropathicpain), etiology (eg, arthritis
or cancer pain), or the affected area (eg, headache or low back pain). Such
classifications are useful in the selection of treatmentmodalities and drug
therapy. Nociceptive pain is caused by activation or sensitization ofperipheral
nociceptors, specialized receptors that transduce noxious stimuli. Neuropathic
pain is the result of injury or acquired abnormalities of periph-eral or
central neural structures.
There are differences in pain perception related to gender and age.
Research has confirmed differ-ences in pain experiences
and coping strategies between genders, and there is ongoing investigation into
exactly how this processing differs. Brain activa-tion differs between genders,
with men particularly influenced by the type and intensity of a noxious
stimulus. Brain imaging patterns differ as well. Some of these differences
decrease with age and may dis-appear after age 40.
A. Acute Pain
Acute pain is caused by noxious stimula-tion
due to injury, a disease process, or theabnormal function of muscle or viscera.
It is usu-ally nociceptive. Nociceptive pain serves to detect, localize, and
limit tissue damage. Four physiologi-cal processes are involved: transduction, transmis-sion,
modulation, and perception. This type of pain is typically associated with a
neuroendocrine stress response that is proportional to the pain’s intensity.
Its most common forms include post-traumatic, postoperative, and obstetric pain
as well as pain associated with acute medical illnesses, such as myo-cardial
infarction, pancreatitis, and renal calculi. Most forms of acute pain are
self-limited or resolve with treatment in a few days or weeks. When pain fails
to resolve because of either abnormal healing or inadequate treatment, it
becomes chronic (below). Two types of acute (nociceptive) pain—somatic and
visceral—are differentiated based on origin and features.
1.Somatic pain—Somatic pain can be further clas-sified as superficial or deep. Superficial somatic pain is due to nociceptive input arising from skin, subcu-taneous tissues, and mucous membranes. It is char-acteristically well localized and described as a sharp, pricking, throbbing, or burning sensation.
Deep somatic pain arises from muscles, ten-dons, joints, or bones. In
contrast to superficial somatic pain, it usually has a dull, aching quality and
is less well localized. An additional feature is that both the intensity and
duration of the stimulus affect the degree of localization. For example, pain
following brief minor trauma to the elbow joint is localized to the elbow, but
severe or sustained trauma often causes pain in the whole arm.
2. Visceral pain—Visceral acute pain is due to adisease process or abnormal function
involving an internal organ or its covering (eg, parietal pleura, pericardium,
or peritoneum). Four subtypes are de-scribed: (1) true localized visceral pain,
(2) localized parietal pain, (3) referred visceral pain, and (4) re-ferred
parietal pain. True visceral pain is dull, diffuse, and usually midline. It is
frequently associated with abnormal sympathetic or parasympathetic activity
causing nausea, vomiting, sweating, and changes in blood pressure and heart
rate. Parietal pain is typi-cally sharp and often described as a stabbing
sensa-tion that is either localized to the area around the organ or referred to
a distant site ( Table 47–2).
The phenomenon of visceral or parietal pain referred to cutaneous areas results
from patterns of embryolog-ical development and migration of tissues, and the
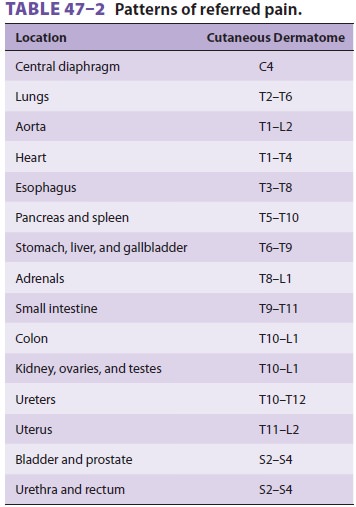
convergence of visceral and somatic afferent input into the central
nervous system. Thus, pain associat-ed with disease processes involving the
peritoneum or pleura over the central diaphragm is frequently referred to the
neck and shoulder, whereas pain from disease processes affecting the parietal
surfaces of the peripheral diaphragm is referred to the chest or upper
abdominal wall.
B. Chronic Pain
Chronic pain is pain that persists beyond the
usual course of an acute disease or aftera reasonable time for healing to
occur; this heal-ing period typically can vary from 1 to 6 months. Chronic pain
may be nociceptive, neuropathic, or mixed. A distinguishing feature is that
psychologi-cal mechanisms or environmental factors frequently play a major
role. Patients with chronic pain often have attenuated or absent neuroendocrine
stress responses and have prominent sleep and affective (mood) disturbances.
Neuropathic pain is classically paroxysmal and lancinating, has a burning
quality, and is associated with hyperpathia. When it is also associated with
loss of sensory input (eg, amputa-tion) into the central nervous system, it is
termed deafferentation pain. When the
sympathetic systemplays a major role, it is often termed sympatheticallymaintained pain.
The most common forms of chronic pain include
those associated with musculoskeletal disor-ders, chronic visceral disorders,
lesions of peripheral nerves, nerve roots, or dorsal root ganglia (including
diabetic neuropathy, causalgia, phantom limb pain, and postherpetic neuralgia),
lesions of the central nervous system (stroke, spinal cord injury, and
mul-tiple sclerosis), and cancer pain. The pain of most musculoskeletal
disorders (eg, rheumatoid arthritis and osteoarthritis) is primarily
nociceptive, whereas pain associated with peripheral or central neural
disorders is primarily neuropathic. The pain asso-ciated with some disorders,
eg, cancer and chronic back pain (particularly after surgery), is often mixed.
Some clinicians use the term chronic
benign pain when pain does not result from cancer. This termi-nology should
be discouraged, however, because pain is never benign from the patient’s point
of view, regardless of its cause.
Related Topics