Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Eye and Vision Disorders
Surgical Procedures and Enucleation - Eye and Vision Disorders
Surgical Procedures and
Enucleation
ORBITAL SURGERIES
Orbital
surgeries may be performed to repair fractures, remove a foreign body, or
remove benign or malignant growths. Surgical procedures involving the orbit and
lids affect facial appearance (ie, cosmesis). The goals are to recover and
preserve visual func-tion and to maintain the anatomic relationship of the
ocular structures to achieve cosmesis. During the repair of orbital frac-tures,
the orbital bones are realigned to follow the anatomic positions of facial
structures.
Orbital
surgical procedures involve working around delicate structures of the eye, such
as the optic nerve, retinal blood vessels, and ocular muscles. Complications of
orbital surgical procedures may include blindness as a result of damage to the
optic nerve and its blood supply. Sudden pain and loss of vision may indicate
in-traorbital hemorrhage or compression of the optic nerve. Ptosis and diplopia
may result from trauma to the extraocular muscles during the surgical
procedure, but these conditions typically re-solve after a few weeks.
Postoperative Management
Prophylaxis with intravenous antibiotics is the
usual postopera-tive regimen after orbital surgery, especially with repair of
orbital fractures and intraorbital foreign body removal. Intravenous
cor-ticosteroids are used if there is a concern about optic nerve swelling.
Topical ocular antibiotics are typically instilled, and an-tibiotic ointments
are applied externally to the skin suture sites.
For the first 24 to 48 hours postoperatively, ice
compresses are applied over the periocular area to decrease periorbital
swelling, facial swelling, and hematoma. The head of the patient’s bed should
be elevated to a comfortable position (30 to 45 degrees).
Discharge
teaching should include medication instructions for oral antibiotics,
instillation of ophthalmic medications, and ap-plication of ocular compresses.
ENUCLEATION
Enucleation
is the removal of the entire eye and part of the optic nerve. It may be performed
for the following conditions:
·
Severe injury resulting in
prolapse of uveal tissue or loss of light projection or perception
·
An irritated, blind, painful,
deformed, or disfigured eye, usually caused by glaucoma, retinal detachment, or
chronic inflammation
·
An eye without useful vision
that is producing or has pro-duced sympathetic ophthalmia in the other eye
·
Intraocular tumors that are
untreatable by other means
The
procedure for enucleation involves the separation and cutting of each of the
ocular muscles, dissection of the Tenon’s capsule (ie, fibrous membrane
covering the sclera), and the cut-ting of the optic nerve from the eyeball. The
insertion of an or-bital implant typically follows, and the conjunctiva is
closed. A large pressure dressing is applied over the area.
Evisceration involves
the surgical removal of the intraocularcontents through an incision or opening
in the cornea or sclera. The optic nerve, sclera, extraocular muscles, and
sometimes, thecornea are left intact. The main advantage of evisceration over
enucleation is that the final cosmetic result and motility after fit-ting the
ocular prosthesis are enhanced. This procedure would be more acceptable to a
patient whose concept of the alteration of body image is severely threatened. The
main disadvantage is the high risk of sympathetic ophthalmia.
Exenteration is
the removal of the eyelids, the eye, and vari-ous amounts of orbital contents.
It is indicated in malignancies in the orbit that are life threatening or when
more conservative modalities of treatment have failed or are inappropriate. An
ex-ample is squamous cell carcinoma of the paranasal sinuses, skin, and
conjunctiva with deep orbital involvement. In its most ex-tensive form,
exenteration may include the removal of all orbital tissues and resection of
the orbital bones.
Ocular Prostheses
Orbital
implants and conformers (ie, ocular prostheses usually made of silicone rubber)
maintain the shape of the eye after enu-cleation or evisceration to prevent a
contracted sunken appear-ance. The temporary conformer is placed over the
conjunctival closure after the implantation of an orbital implant. A conformer
is placed after the enucleation or evisceration procedure to pro-tect the
suture line, maintain the fornices, prevent contracture of the socket in
preparation for the ocular prosthesis, and promote the integrity of the
eyelids.
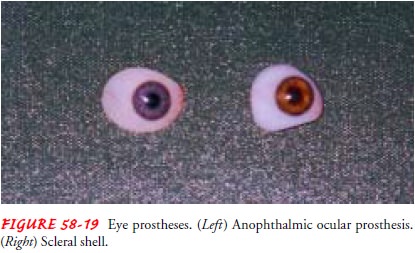
All ocular prosthetics have limitations in their
motility. There are two designs of eye prostheses. The anophthalmic ocular
pros-theses are used in the absence of the globe. Scleral shells look just like
the anophthalmic prosthesis (Fig. 58-19) but are thinner and fit over a globe
with intact corneal sensation. An eye prosthesis usually lasts about 6 years,
depending on the quality of fit, com-fort, and cosmetic appearance. When the
anophthalmic socket is completely healed, conformers are replaced with
prosthetic eyes.
An ocularist is a specially trained and skilled
professional who makes prosthetic eyes. After the ophthalmologist is satisfied
that the anophthalmic socket is completely healed and is ready for prosthetic
fitting, the patient is referred to an ocularist. The heal-ing period is
usually 6 to 8 weeks. It is advisable for the patient to have a consultation
with the ocularist before the fitting. Obtain-ing accurate information and
verbalizing concerns can lessen anx-iety about wearing an ocular prosthesis.
Medical Management
Removal
of an eye has physical, social, and psychological rami-fications for any
person. The significance of loss of the eye and vision must be addressed in the
plan of care. The patient’s prep-aration should include information about the
surgical procedure and placement of orbital implants and conformers and the
avail-ability of ocular prosthetics to enhance cosmetic appearance. In some
cases, patients may choose to see an ocularist before the surgery to discuss
ocular prosthetics.
Nursing Management
TEACHING ABOUT POSTSURGICAL AND PROSTHETIC CARE
Patients who undergo eye removal need to know that they will usually have a large ocular pressure dressing, which is typically removed after a week, and that an ophthalmic topical antibiotic ointment is applied in the socket three times daily.
After the removal of an eye, there is a loss of
depth perception. Patients must be advised to take extra caution in their
ambula-tion and movement to avoid miscalculations that may result in injury. It
may take some time to adjust to monocular vision.
The
patient must be advised that conformers may accidentally fall out of the
socket. If this happens, the conformer must be washed, wiped dry, and placed
back in the socket. When surgical eye removal is unexpected, such as in severe
ocular trauma, leav-ing no time for the patient and family to prepare for the
loss, the nurse’s role in providing reassurance and emotional support is
crucial.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care.Patients need to be taught how toinsert, remove, and care for the
prosthetic eye. Proper hand wash-ing must be observed before inserting and
removing an ocular prosthesis. A suction cup may be used if there are problems
with manual dexterity. Precautions, such as draping a towel over the sink and
closing the sink drain, must be taken to avoid loss of the prosthesis. When instructing
patients or family members, a re-turn demonstration is important to assess the
level of under-standing and ability to perform the procedure.
Before
insertion, the inner punctal or outer lateral aspects and the superior and
inferior aspects of the prosthesis must be identi-fied by locating the
identifying marks, such as a reddish color in the inner punctal area. For
people with low vision, other forms of identifying markers, such as dots or
notches, are used. The upper lid is raised high enough to create a space; then
the patient learns to slide the prosthesis up, underneath, and behind the upper
eyelid. Meanwhile, the patient pulls the lower eyelid down to help put the
prosthesis in place and to have its inferior edge fall back gradually to the lower
eyelid. The lower eyelid is checked for correct positioning.
To remove the prosthesis, the patient cups one hand
on the cheek to catch the prosthesis, places the forefinger of the free hand
against the midportion of the lower eyelid, and gazes upward. Gazing upward
brings the inferior edge of the prosthesis nearer the inferior eyelid margin.
With the finger pushing inward, downward, and laterally against the lower
eyelid, the prosthesis slides out, and the cupped hand acts as the receptacle.
Continuing Care.An eye prosthesis can be worn
and left in placefor several months. Hygiene and comfort are usually maintained
with daily irrigation of the prosthesis in place with the use of abalanced salt solution, hard contact lens solution,
or artificial tears. In the case of dry eye symptoms, the use of ophthalmic
ointment lubricants or oil-based drops, such as vitamin E and mineral oil, can
be helpful. Removing crusting and mucous discharge that accumulates overnight
is performed with the prosthesis in place. Malpositions may occur when wiping
or rubbing the prosthesis in the socket. The prosthesis can be turned back in
place with the use of clean fingers. Proper wiping of the prosthesis should be
a gentle temporal-to-nasal motion to avoid malpositions.
The
prosthesis needs to be removed and cleaned when it be-comes uncomfortable and
when there is increased mucous dis-charge. The socket should also be rendered
free of mucus and inspected for any signs of infection. Any unusual discomfort,
irritation, or redness of the globe or eyelids may indicate exces-sive wear,
debris under the shell, or lack of proper hygiene. Any infection or irritation
that does not subside needs medical attention.
Related Topics