Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Eye and Vision Disorders
Corneal Disorders
Corneal Disorders
CORNEAL DYSTROPHIES
Corneal dystrophies are inherited as autosomal dominant traits and manifest when the person is about 20 years of age. They are characterized by deposits in the corneal layers.
Decreased vision is
caused by the irregular corneal surface and corneal deposits. Corneal
endothelial decompensation leads to corneal edema and blurring of vision.
Persistent edema leads to bullous
keratopathy, which is formation of blisters that cause pain and discomfort
on rupturing. This condition is usually associated with primary open-angle
glaucoma.
A
bandage contact lens is used to flatten the bullae, protect the exposed corneal
nerve endings, and relieve discomfort. Sympto-matic treatments, such as
hypertonic drops or ointment (5% sodium chloride), may reduce epithelial edema;
lowering the IOP also reduces stromal edema. Penetrating keratoplasty has a
high success rate in advanced cases (see “Corneal Surgeries”). For dif-fuse
bullous keratopathy, amniotic membrane transplantation may become the procedure
of choice for patients with limited visual potential (Rapuano, 2000).
KERATOCONUS
Keratoconus is
a condition characterized by a conical protuber-ance of the cornea with
progressive thinning on protrusion and irregular astigmatism. The hereditary
condition has a higher in-cidence among women. Onset occurs at puberty; the
condition may progress for more than 20 years and is bilateral. Corneal
scarring occurs in severe cases. Blurred vision is a prominent symptom. Rigid,
gas-permeable contact lenses correct irregular astigmatism and improve vision.
Advances in contact lens de-sign have reduced the need for surgery. Penetrating
kerato-plasty is indicated when contact lens correction is no longer effective.
CORNEAL SURGERIES
Among the surgical procedures used to treat
diseased corneal tis-sue are phototherapeutic keratectomy (PTK) and
keratoplasty.
Phototherapeutic Keratectomy
PTK is a laser procedure that is used to treat
diseased corneal tis-sue by removing or reducing corneal opacities and
smoothing the anterior corneal surface to improve functional vision. PTK is a
safer, more effective (when indicated) alternative than penetrat-ing or
lamellar keratoplasty. PTK is contraindicated in patients with active herpetic
keratitis because the ultraviolet rays may re-activate latent virus. Common
side effects are induced hyperopia and stromal haze. Complications are delayed
re-epithelialization (particularly in patients with diabetes) and bacterial
keratitis. Postoperative management consists of oral analgesics for eye pain.
Re-epithelialization is promoted with a pressure patch or thera-peutic soft
contact lens. Antibiotic and corticosteroid ointment and NSAIDs are prescribed
postoperatively. Follow-up examina-tions are required for up to 2 years.
Keratoplasty
Keratoplasty
(ie, corneal transplantation or corneal grafting) involves replacing abnormal
host tissue with a healthy donor corneal tissue. Common indications are
keratoconus, corneal dystrophy, corneal scarring from herpes simplex keratitis,
and chemical burns.
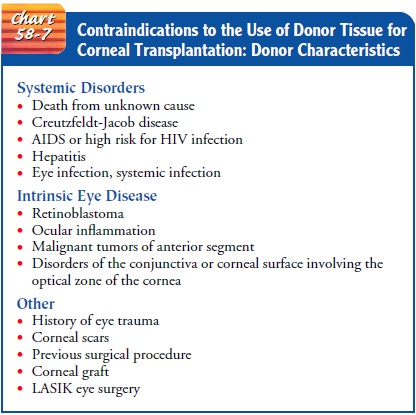
Several factors affect the success of the graft:
ocular structures (eg, lids, conjunctiva), tear film function, adequacy of
blinking, and viability of the donor endothelium. Tissue that is the possi-ble
source of disease transmission from donor to recipient orcornea with
functionally compromised endothelium is typically not used for grafting (Chart
58-7), nor is corneal tissue used from donors who have undergone laser-assisted
in situ keratomileusis (LASIK) because the cornea is no longer intact. Conditions
such as glaucoma, retinal disease, and strabismus
(ie, deviation in oc-ular alignment) can negatively influence the outcome.
Promising experimental therapies include stem cell transplants (Rongé, 2001)
and autologous limbal epithelial cell transplants (Tsai et al., 2000).
The surgeon determines the graft size before the
procedure, and the appropriate size is marked on the surface of the cornea. The
surgeon prepares the donor cornea and the recipient bed, re-moves the diseased
cornea, places the donor cornea on the recip-ient bed, and sutures it in place.
Sutures remain in place for 12 to 18 months. Potential complications include
early graft failure due to poor quality of donor tissue, surgical trauma, acute
in-fection, and persistently increased IOP and late graft failure due to
rejection.
Postoperatively, the patient receives mydriatic
medications (2 weeks) and topical corticosteroids (12 months; daily doses formonths
and tapered doses thereafter). Patients typically de-scribe a sensation of
postoperative eye discomfort rather than acute pain.
Nursing Management
The nurse reinforces the surgeon’s recommendations and in-structions regarding visual rehabilitation and visual improvement by explaining why a technically successful graft may initially pro-duce disappointing results because the procedure has produced a new optical surface and only after several months do patients start seeing the natural and true colors of their environment. Correc-tion of a resultant refractive error with eyeglasses or contact lenses determines the final visual outcome. The nurse assesses the pa-tient’s support system and his or her ability to comply with long-term follow-up, which includes frequent clinic visits for several months for tapering of topical corticosteroid therapy, selective suture removal, and ongoing evaluation of the graft site and visual acuity. The nurse also initiates appropriate referral to community services when indicated.
Because graft failure is an ophthalmic emergency
that can occur at any time, the primary goal of nursing care is to teach the
patient to identify signs and symptoms of graft failure. The early symptoms are
blurred vision, discomfort, tearing, or redness of the eye. Decreased vision
results after graft destruction. Patients must contact the ophthalmologist as
soon as symptoms occur. Treatment of graft rejection is prompt administration
of hourly topical corticosteroids and periocular corticosteroid injections.
Systemic immunosuppressive agents may be necessary for severe, resistant cases.
REFRACTIVE SURGERIES
Refractive
surgeries are cosmetic, elective procedures performed to reshape corneal tissue
and correct refractive errors so that eye-glasses or contact lenses are no
longer needed. Current procedures include radial keratotomy, photorefactive
keratectomy (PFK), and LASIK.
Refractive
surgery alters the major optical function of the eye and thereby carries
certain surgical risks. The patient must fully understand benefits, potential
risks and complications, common side effects, and limitations of the procedure.
Refractive surgery does not alter the normal aging process of the eye. If the
reason for the procedure is occupational vision requirements, the results must
satisfy both the patient and the employer. Precise visual out-come cannot be
guaranteed with certainty. Typically, patients must be at least 18 years of
age.
The corneal structure must be normal and refractive
error sta-ble. Patients are required to discontinue using contact lenses for a
period before the procedure (ie, 2 to 3 weeks for soft lenses and 4 weeks for
hard lenses). Patients with conditions that are likely to adversely affect
corneal wound healing (eg, corticosteroid use, immunosuppression, elevated IOP)
are not good candidates for the procedure. Any superficial eye disease must be
diagnosed and fully treated before a refractive procedure.
Radial Keratotomy
Radial keratotomy (RK) is indicated for low myopia
(less than 8D). The procedure involves making four to eight, deep, radial
incisions in the paracentral and peripheral cornea with a metal or diamond
blade. The corneal contour then becomes flatter. Glare, photosensitivity,
fluctuations of vision during the day, and occa-sional diplopia are common side
effects. As the popularity of laser refractive surgery grows, RK procedures
decrease.
Laser Vision Correction Photorefractive Keratectomy
Laser vision correction photorefractive keratectomy
(PRK) is a procedure used to treat myopia and hyperopia with or without
astigmatism. The 193-mm argon fluoride excimer laser is ap-plied directly to
the cornea according to carefully calculated measurements. For myopia, the
relative curvature is decreased; for hyperopia, the relative curvature is
increased. A bandage con-tact lens is placed over the cornea to promote
epithelial healing and reduce pain similar to that of severe corneal abrasion.
PRK requires a longer visual recovery period than RK, but PRK pro-vides more
predictable and stable results. Except for the side effect of corneal haze and
night vision problems, PRK has not been associated with the two major
disadvantages of RK: hyper-opic drift and weakening of the structural integrity
of the cornea.
Laser-Assisted In Situ Keratomileusis (LASIK)
An
improvement over PRK, particularly for correcting high (severe) myopia, LASIK
involves flattening the anterior curvature of the cornea by removing a stromal
lamella or layer. The surgeon creates a corneal flap with a microkeratome,
which is an auto-matic corneal shaper similar to a carpenter’s plane. The surgeon
retracts a flap of corneal tissue less than one third of the thickness of a
human hair to access the corneal stroma and then uses the ex-cimer laser on the
stromal bed to reshape the cornea according to calculated measurements (Fig.
58-10). The corneal flap, a natu-rally adhering bandage, is rolled back and
repositioned. LASIK also appears to be an effective, predictable, stable, and
safe pro-cedure for correcting residual myopia after cataract surgery (Ayala et
al., 2001).
LASIK causes less postoperative discomfort, has
fewer side ef-fects, and is safer than PRK. The patient has no corneal haze and
requires less postoperative care. With LASIK, however, the cornea has been
invaded at a deeper level, and any complications are more significant than those
that can occur with PRK.
PERIOPERATIVE COMPLICATIONS
Ablation-Related
Complications.Ablation complications ofLASIK include an elevated
area within the corneal treatment ab-lation zone (ie, central island). Signs
and symptoms of this com-plication include ghosting, blurred vision, halo
formation around lights, decreased visual activity, and contrast sensitivity in
low light. Most of the island formations resolve over time; reablation is
considered only after the island appears stable after repeated examinations for
at least 3 months.
Diffuse Lamellar Keratitis. As LASIK increases in popularity andis performed more often, the vision-threatening complication known as diffuse lamellar keratitis (DLK) is reported more often. DLK is a peculiar, noninfectious, inflammatory reaction in the lamellar interface after LASIK. DLK is characterized by a white, granular, diffuse, culture-negative lamellar keratitis occurring in the first week after surgery. Studies suggest that, because no sin-gle agent appears to be solely the cause of DLK, the cause is multi-factorial (Holland et. al., 2000).
DLK is diagnosed by identifying cells in the
lamellar interface by slit-lamp examination from postoperative day 1. Depending
on the severity of the condition, treatment methods range from administering
corticosteroid drops to intervening surgically.
Central Islands and Decentered
Ablations.Decentered or ec-centric ablation involves a shift
of the center of the ablation pat-tern from the pupil or visual axis to a more
eccentric location. Symptoms include decreased visual acuity, halos, glare, and
ghosting, especially in low-light settings.
LASIK Enhancements
LASIK
enhancements are surgical options from improved tech-nology and software used
to treat a wider range of myopia, hyper-opia, and astigmatism in eyes with a
history of LASIK surgery. Astigmatic keratotomy continues to work well for
patients with significant regular astigmatism. A newer procedure, Intacs
im-plantation, is performed for patients left with significant myopia but who
have thin corneas. Hyperopic excimer laser enhance-ments are indicated for
patients who have undergone myopic LASIK and have consecutive hyperopia.
IMPLANTABLE DEVICES
Because
the results of refractive surgery on high (severe) myopia, hyperopia, and
astigmatism are less predictable, there has been in-creasing interest in the
use of phakic IOLs. Anterior and poste-rior chamber IOLs are now in use, and
design improvements continue to be made. Phakic IOL implantation does not
com-promise the central optical zone and retains the normal aspheric contour of
the cornea. Most importantly, it is reversible. Early re-search results on
vision quality favor phakic IOL over LASIK. Po-tential complications include
cataract, iritis or uveitis, endothelial cell loss, and increased IOP.
Intacs
is an implantable intrastromal corneal ring used to cor-rect mild to moderate
myopia. The intrastromal corneal ring seg-ments are placed in the corneal
stroma outside of the central optical zone and reshape the anterior surface of
the cornea.
Management
Patient satisfaction is the ultimate goal;
therefore, patient educa-tion and counseling about potential risks,
complications, and postoperative follow-up are critical. Minimal postoperative
care includes topical corticosteroid drops. The length of postoperative
follow-up depends on the refractive procedure, with PRK re-quiring a longer
course, followed by RK and then LASIK.
Related Topics