Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Eye and Vision Disorders
Ocular Trauma
OCULAR TRAUMA
Ocular
trauma is the leading cause of blindness among children and young adults,
especially male trauma victims. The most com-mon circumstances of ocular trauma
are occupational injuries (eg, construction industry), sports (eg, baseball,
basketball, racket sports, boxing), weapons (eg, air guns, BB guns), assault,
motor vehicle crashes (eg, broken windshields), and war (eg, blast fragments).
For
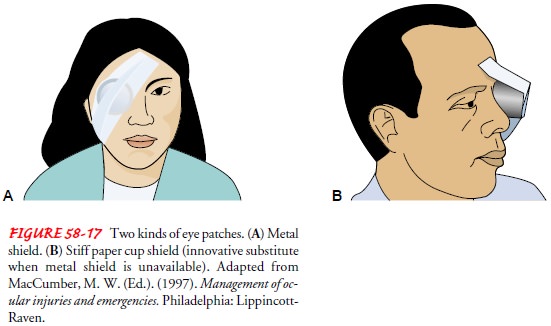
the nonophthalmic practitioner, initial intervention is performed in only two
conditions: chemical burns, for which irrigation of the eye with normal saline
solution or even plain tap water must occur immediately, and a foreign body, for
whichabsolutely no attempt is made to remove the foreign material, small or
big, or apply pressure or patch to the injured eye. The eye must be protected
using a metal shield, if available, or a stiff paper cup (Fig. 58-17). All
traumatic eye injuries should be properly shielded.
Assessment and Diagnostic Findings
A
thorough history is obtained, particularly assessing the patient’s ocular
history, such as preinjury vision in the affected eye or past ocular surgery.
Details related to the injury that help in the diag-nosis and assessment of
need for further tests include the nature of the ocular injury (ie, blunt or
penetrating trauma), the type of activity causing the injury to determine the
nature of the force striking the eye, and whether onset of vision loss was
sudden, slow, or progressive. For chemical eye burns, the chemical agent must
be identified and tested for pH if a sample is available. The corneal surface
is examined for foreign bodies, wounds, and abra-sions, after which the other
external structures of the eye are ex-amined. Pupillary size, shape, and light
reaction of the pupil of the affected eye are compared with the other eye.
Ocular motil-ity, which is the ability of the eyes to move synchronously up,
down, right, and left, is also assessed.
Medical Management
SPLASH INJURIES
Splash injuries are irrigated with normal saline
solution before further evaluation. In cases of ruptured globe, cycloplegic
agents (ie, agents that paralyze the ciliary muscle) or topical antibiotics
must be deferred because of potential toxicity to exposed intra-ocular tissues.
Further manipulation of the eye must be avoided until the patient is under
general anesthesia. Parenteral, broad-spectrum antibiotics are initiated.
Tetanus antitoxin is adminis-tered, if indicated, as well as analgesics.
(Tetanus prophylaxis is recommended for full-thickness ocular and skin wounds.)
Any topical medication (eg, anesthetic, dyes) must be sterile.
FOREIGN BODIES AND CORNEAL ABRASIONS
After removal of a foreign body from the surface of
the eye, an antibiotic ointment is applied, and the eye is patched. The eye is
examined daily for evidence of infection until the wound is com-pletely
healed.Contact lens wear is a common cause of corneal abrasion. The patient
experiences severe pain and photophobia
(ie, ocular pain on exposure to light).
Corneal epithelial defects are treated with
antibiotic ointment and a pressure patch to immobilize the eye-lids. It is of
utmost importance that topical anesthetic eye drops are not given to a patient
for repeated use after corneal injury be-cause their effects mask further
damage, delay healing, and can lead to permanent corneal scarring.
Corticosteroids are avoided while the epithelial defect exists.
Penetrating Injuries and Contusions of the Eyeball
Sharp penetrating injury or blunt contusion force
can rupture the eyeball. When the eye wall, cornea, and sclera rupture, rapid
de-compression or herniation of the orbital contents into adjacent sinuses can
occur. In general, blunt traumatic injuries (with an increased incidence of
retinal detachment, intraocular tissue avul-sion, and herniation) have a worse
prognosis than penetrating in-juries. Most penetrating injuries result in
marked loss of vision with the following signs: hemorrhagic chemosis (ie, edema of the
conjunctiva), conjunctival laceration, shallow anterior chamber with or without
an eccentrically placed pupil, hyphema
(ie, hem-orrhage within the chamber), or vitreous hemorrhage.
Hyphema is caused by contusion forces that tear the
vessels of the iris and damage the anterior chamber angle. Preventing
re-bleeding and prolonged increased IOP are the goals of treatment for hyphema.
In severe cases in which patient compliance is ques-tionable, the patient is
hospitalized with moderate activity re-striction. An eye shield is applied.
Topical corticosteroids are prescribed to reduce inflammation. An
antifibrinolytic agent, aminocaproic acid (Amicar), stabilizes clot formation
at the site of hemorrhage. Aspirin is contraindicated.
A ruptured globe and severe injuries with
intraocular hemor-rhage require surgical intervention. Vitrectomy is performed
for traumatic retinal detachments. Primary enucleation
(ie, com-plete removal of the eyeball and part of the optic nerve) is
con-sidered only if the globe is irreparable and has no light perception. It is
a general rule that enucleation is performed within 2 weeks of the initial
injury (in an eye that has no useful vision after sus-taining penetrating
injury) to prevent the risk of sympatheticophthalmia,
an inflammation created in the fellow eye by theaffected eye that can
result in blindness of the fellow eye.
Intraocular Foreign Bodies
A patient who complains of blurred vision and
discomfort should be questioned carefully about recent injuries and exposures.
Patients may be injured in a number of different situations and suffer an
intraocular foreign body (IOFB). Precipitating cir-cumstances can include
working in construction, striking metal against metal, being involved in motor
vehicle crashes with facial injury, gunshot wounds, and grinding-wheel work.
IOFB is diagnosed and localized by slit-lamp biomicroscopy and indirect ophthalmoscopy, as well as CT or ultrasonography. MRI is contraindicated because most foreign bodies are metallic and magnetic.
It is important to determine the composition, size, and location of
the IOFB and affected eye structures. Every effort should be made to identify
the type of IOFB and whether it is magnetic. Iron, steel, copper, and vegetable
matter cause intense inflammatory reactions. The incidence of endophthalmitis
is also high. If the cornea is perforated, tetanus prophylaxis and intra-venous
antibiotics are administered. The extraction route (ie, sur-gical incision) of
the foreign body depends on its location and composition and associated ocular
injuries. Specially designed IOFB forceps and magnets are used to grasp and
remove the for-eign body. Any damaged area of the retina is treated to prevent
retinal detachment.
Related Topics