Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Eye and Vision Disorders
Concepts in Ocular Medication Administration
Concepts in Ocular Medication
Administration
The main objective of ocular medication delivery is
to maximize the amount of medication that reaches the ocular site of action in
sufficient concentration to produce a beneficial therapeutic effect. This is
determined by the dynamics of ocular pharmacokinetics: absorption,
distribution, metabolism, and excretion.
Topical
administration of ocular medications results in only a 1% to 7% absorption rate
by the ocular tissues. Ocular absorp-tion involves the entry of a medication
into the aqueous humor through the different routes of ocular drug administration.
The rate and extent of aqueous humor absorption are determined by the
characteristics of the medication and the barriers imposed by the anatomy and
physiology of the eye. The natural barriers of absorption that diminish the
efficacy of ocular medications in-clude the following:
·
Limited
size of the conjunctival sac. The conjunctival sac canhold
only 50 μ L,
and any excess is wasted. The volume of one eye drop from commercial topical
ocular solutions typ-ically ranges from 20 to 35 μ L.
·
Corneal
membrane barriers. The epithelial, stromal,
andendothelial layers are barriers to absorption.
·
Blood–ocular
barriers. Blood–ocular barriers prevent highocular tissue
concentration of most ophthalmic medications because they separate the
bloodstream from the ocular tis-sues and keep foreign substances from entering
the eye, thereby limiting a medication’s efficacy.
·
Tearing,
blinking, and drainage. Increased tear productionand
drainage due to ocular irritation or an ocular condition may dilute or wash out
an instilled eye drop; blinking ex-pels an instilled eye drop from the
conjunctival sac.
Distribution
of an ocular medication into the ocular tissues in-volves partitioning and
compartmentalizing of the medication between the tissues of the conjunctiva,
cornea, lens, iris, ciliary body, choroid, and vitreous. Medications penetrate
the corneal epithelium by diffusion by passing through the cells
(intracellu-lar) or by passing between the cells (intercellular). Water-soluble
(hydrophilic) medications diffuse through the intracellular route, and
fat-soluble (lipophilic) medications diffuse through the in-tercellular route.
Topical administration usually does not reach the retina in significant
concentrations. Because the space be-tween the ciliary process and the lens is
small, medication diffu-sion in the vitreous is slow. When high therapeutic
medication concentration in the vitreous is required, intraocular injection is
often chosen to bypass the natural ocular anatomic and physi-ologic barriers.
Aqueous solutions are most commonly used for the
eye. They are the least expensive medications and interfere least with vision.
However, corneal contact time is brief because tears dilute the medication.
Ophthalmic ointments have extended retention time in the conjunctival sac and a
higher concentration than eye drops. The major disadvantage of ointments is the
blurred vision that results after application. In general, eyelids and eyelid
margins are best treated with ointments. The conjunctiva, limbus, cornea, and
anterior chamber are treated most effectively with instilled solutions or
suspensions. Subconjunctival injection may be nec-essary for better absorption
in the anterior chamber. If high medication concentrations are required in the
posterior chamber, in-travitreal injections or systemically absorbed
medications are con-sidered. Contact lenses and collagen shields soaked in
antibiotics are alternative delivery methods for treating corneal infections.
Of all these delivery methods, the topical route of administra-tion—instilled
eye drops and applied ointments—remain the most common. Topical instillation,
which is the least invasive method, permits self-administration of medication.
It also pro-duces fewer side effects.
Preservatives are commonly used in ocular
medications. Ben-zalkonium chloride, for example, prevents the growth of
organ-isms and enhances the corneal permeability of most medications. Some
patients are allergic to this preservative. This may be sus-pected even if the
patient had never before experienced an aller-gic reaction to systemic use of
the medication in question. Eye drops without preservatives can be prepared by
pharmacists.
COMMONLY USEDOCULAR MEDICATIONS
Common
ocular medications include topical anesthetic, mydri-atic, and cycloplegic
agents that reduce IOP; anti-infective med-ications, corticosteroids, NSAIDS,
antiallergy medications, eye irrigants, and lubricants.
Topical Anesthetics
One to two drops of proparacaine hydrochloride
(Ophthaine 0.5%) and tetracaine hydrochloride (Pontocaine 0.5%) are instilled
before diagnostic procedures such as tonometry and gonioscopy and in minor
ocular procedures such as removal of sutures or con-junctival or corneal
scrapings. The nurse must instruct patients not to rub their eyes while
anesthetized because this may result in corneal damage. Patients must never be
allowed to take topical anesthetics home. Prolonged use can delay wound healing
and can lead to permanent corneal opacification and scarring, result-ing in
visual loss. Topical anesthetic is also used for severe eye pain to allow the
patient to open his or her eyes for examination or treatment (eg, eye irrigation
for chemical burns). Anesthesia occurs within 20 seconds to 1 minute and lasts
10 to 20 minutes.
Mydriatics and Cycloplegics
Mydriasis,
or pupil dilation, is the main objective of the adminis-tration of mydriatic
and cycloplegic agents (Table 58-8). These two medications function differently
and are used in combination to achieve the maximal dilation that is needed
during surgery and fundus examinations to give the ophthalmologist a better
view of the internal eye structures. Mydriatics potentiate alpha-adrenergic
sympathetic effects that result in the relaxation of the ciliary muscle. This
causes the pupil to dilate. This sympathetic action alone, however, is not
enough to sustain mydriasis because of its short duration of action. The strong
light used during an eye examination also stimulates miosis (ie, pupillary
contraction). Cycloplegic medications are administered to paralyze the iris
sphincter.
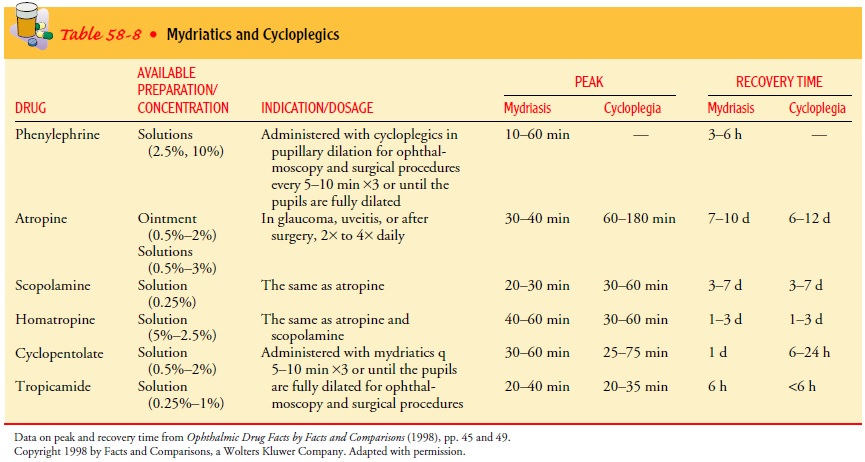
Patients
are instructed about the temporary effects of mydri-asis on vision, such as
glare and the inability to focus properly. Patients may not be able to read and
should not drive. The effects of the various mydriatics and cycloplegics can
last 3 hours to sev-eral days. Patients are advised to wear sunglasses (most
eye clin-ics provide protective sunglasses) and to have a responsible adult
drive them home.
Mydriatic and cycloplegic agents affect the central nervous system. Their effects are most prominent in children and elderly patients; these patients must be assessed closely for symptoms, such as rise in blood pressure, tachycardia, dizziness, ataxia, confusion, disorientation, incoherent speech, and hallucination. These medications are contraindicated in patients with narrow angles or shallow anterior chambers and in patients taking monoamine oxidase inhibitors or tricyclic antidepressants.
Medications Used to Treat Glaucoma
Therapeutic
medications for glaucoma are used to lower IOP by decreasing aqueous production
or increasing aqueous outflow. Because glaucoma calls for lifetime therapy,
patients must be in-structed regarding both the ocular and systemic side
effects of the medications.
Most
antiglaucoma medications affect the accommodation of the lens and limit light
entry through a constricted pupil. Visual acuity and the ability to focus may
be affected. Factors to con-sider in selecting glaucoma medications are
efficacy, systemic and ocular side effects, convenience, and cost.
Anti-Infective Medications
Anti-infective
medications include antibiotic, antifungal, and antiviral agents. Most are
available as drops, ointments, or sub-conjunctival or intravitreal injections.
Antibiotics include peni-cillin, cephalosporins, aminoglycosides, and
fluoroquinolones. The main antifungal agent is amphotericin B. Side effects of
amphotericin are serious and include severe pain, conjunctival necrosis,
iritis, and retinal toxicity. Antiviral medications in-clude acyclovir and
ganciclovir. They are used to treat ocular infections associated with
herpesvirus and CMV. Patients re-ceiving ocular anti-infective agents are
subject to the same side effects and adverse reactions as those receiving oral
or parenteral medications.
Corticosteroids and Nonsteroidal Anti-Inflammatory Drugs
The topical preparations of corticosteroids are
commonly used in inflammatory conditions of the eyelids, conjunctiva, cornea,
an-terior chamber, lens, and uvea. In posterior segment diseases that involve
the posterior sclera, retina, and optic nerve, the topical agents are less
effective, and parenteral and oral routes are pre-ferred. The topical eye drop
preparation is prepared in suspen-sion; the patient is instructed to shake the
bottle several times to obtain the maximum therapeutic effect of the
medication.
The
most common ocular side effects of long-term topical corticosteroid
administration are glaucoma, cataracts, suscepti-bility to infection, impaired
wound healing, mydriasis, and ptosis. High IOP may develop, which is reversible
after cortico-steroid use is discontinued. To avoid the side effects of
cortico-steroids, NSAIDS are used as an alternative in controlling inflammatory
eye conditions and postoperatively to reduce in-flammation. NSAID therapy in
combination with topical and oral preparations is an important adjunct therapy
in managing uveitis.
Antiallergy Medications
Ocular hypersensitivity reactions, such as allergic
conjunctivitis, are extremely common. These conditions result primarily from
responses to environmental allergens. Most allergens are airborne or carried to
the eye by the hand or by other means, although al-lergic reactions may also be
drug induced. Corticosteroids are also commonly used as anti-inflammatory and
immunosuppressive agents to control ocular hypersensitivity reaction.
Ocular Irrigants
Most
irrigating solutions are used to cleanse the external lids to maintain lid
hygiene, to irrigate the external corneal surface to re-gain normal pH (such as
in chemical burns), to irrigate the corneal surface to eliminate debris, or to
inflate the globe intra-operatively. These solutions have various compositions
that in-clude sodium, potassium, magnesium, calcium, bicarbonate, glucose, and
glutathione (ie, substance found in the aqueous humor). Sterile irrigating
solutions, such as Dacriose, for lid hy-giene are available. Irrigating solutions
are safe to use with an in-tact corneal surface; however, the corneal surface
should not be irrigated in cases of threatened corneal perforation. For
patients with severe corneal ulcer, specific orders must be obtained re-garding
whether it is safe to irrigate the corneal surface or just to cleanse the
external lids. Although it is good practice to promote hygiene, prevention of
complications must be the primary con-cern. Normal saline solutions are
commonly used to irrigate the corneal surface when chemical burns occur.
Ocular Lubricants
Lubricants, such as artificial tears, help to
alleviate corneal irritation, such as dry eye syndrome. Artificial tears are
topical preparations of methyl or hydroxypropyl cellulose that are prepared as
eye drop solutions, ointments, or ocular inserts (inserted at the lower
con-junctival cul-de-sac once each day). The eye drops can be instilled as
often as every hour, depending on the severity of symptoms.
NURSING MANAGEMENT
The objectives in administering ocular medications
are to ensure proper administration to maximize the therapeutic effects and to
ensure the safety of the patient by monitoring manifestations of possible
systemic and local side effects. Absorption of eye drops by the nasolacrimal
duct is undesirable because of the potential sys-temic side effects of ocular
medications. To diminish systemic ab-sorption and minimize the side effects, it
is important to occlude the puncta (Chart 58-10). This is especially important
for patients most vulnerable to medication overdose, including elderly people,
children, infants, women who are lactating or are pregnant, and patients with
cardiac, pulmonary, hepatic, or renal disease.
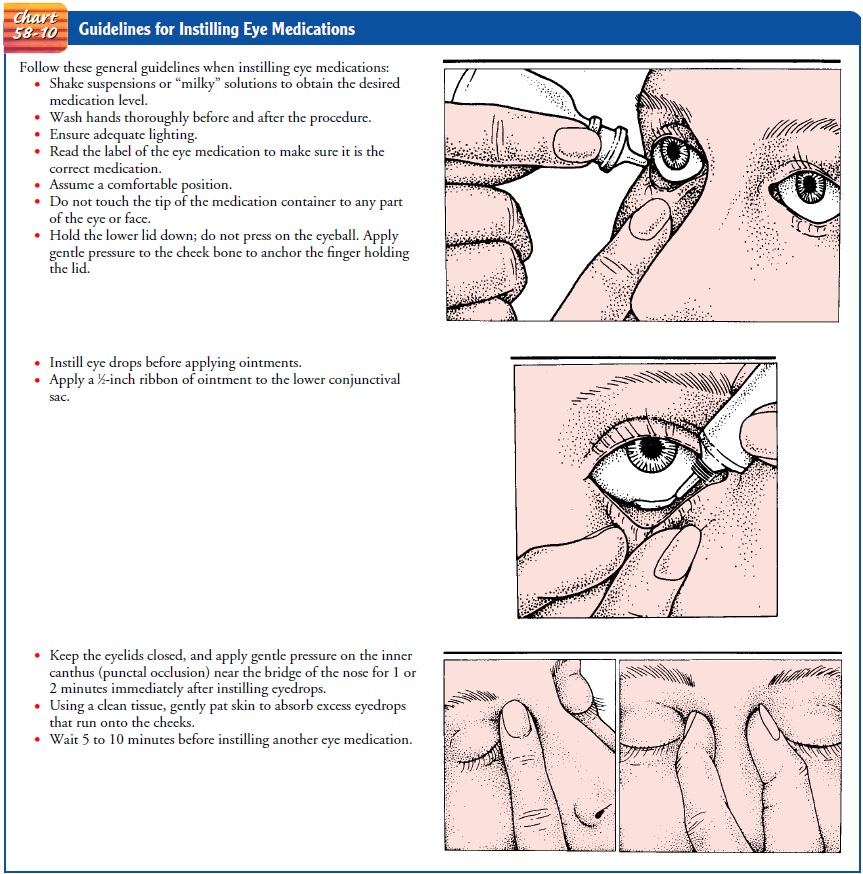
A 30-second interval between eye drop instillations
has a 45% rate of washout loss. A 1-minute interval between instillation of
dif-fering types of ocular drops is recommended (Margolis et al., 2002).
Before
the administration of ocular medications, the nurse should warn the patient
that blurred vision, stinging, and a burn-ing sensation are symptoms that
ordinarily occur after instillation and are temporary. Risk for interactions of
the ocular medication with other ocular and systemic medications must be
emphasized; therefore, a careful patient interview regarding medications being
taken must be obtained.
Emphasis must be placed on hand-washing techniques before and after medication instillation. The tip of the eye drop bottle or the ointment tube must never touch any part of the eye. The medication must be recapped immediately after each use. If pa-tients who instill their own medications cannot feel the eye drops when they are instilled, the eye medication may be refrigerated, because a cold drop is easier to detect. A 5-minute interval be-tween successive eye drop administration allows adequate drug retention and absorption. The patient or the caregiver at home should be asked to demonstrate actual eye drop or ointment instillation and punctal occlusion
Related Topics