Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Eye and Vision Disorders
Conjunctivitis
CONJUNCTIVITIS
Conjunctivitis
(ie, inflammation of the conjunctiva) is the most common ocular disease
worldwide. It is characterized by a pink appearance (hence the common term pink eye) because of sub-conjunctival
blood vessel hemorrhages.
Clinical Manifestations
General
symptoms include foreign body sensation, scratching or burning sensation,
itching, and photophobia. Conjunctivitis may be unilateral or bilateral, but
the infection usually starts in one eye and then spreads to the other eye by
hand contact.
Assessment and Diagnostic Findings
The four main clinical features important to evaluate
are the type of discharge (ie, watery, mucoid, purulent, or mucopurulent), type
of conjunctival reaction (ie, follicular or papillary), presence of
pseudomembranes or true membranes, and presence or absence of lymphadenopathy
(ie, enlargement of the preauricular and submandibular lymph nodes where the
eyelids drain). Pseudomembranes consist of coagulated exudate that adheres to
the surface of the inflamed conjunctiva. True membranes form when the exudate
adheres to the superficial layer of the con-junctiva, and removal results in
bleeding. Follicles are multiple, slightly elevated lesions encircled by tiny
blood vessels; they look like grains of rice. Papillae are hyperplastic
conjunctival epithe-lium in numerous projections that are usually seen as a fine
mo-saic pattern under slit-lamp examination. Diagnosis is based on the
distinctive characteristics of ocular signs, acute or chronic pre-sentation,
and identification of any precipitating events. Positive results of swab smear
preparations and cultures confirm the diagnosis.
Types of Conjunctivitis
Conjunctivitis is classified according to its
cause. The major causes are microbial infection, allergy, and irritating toxic
stimuli. A wide spectrum of exogenous microbes can cause conjunctivitis,
includ-ing bacteria (eg, Chlamydia),
viruses, fungus, and parasites. Con-junctivitis can also result from infection
of an existing ocular infection or can be a manifestation of a systemic
disease.
MICROBIAL CONJUNCTIVITIS
Bacterial
conjunctivitis can be acute or chronic. The acute type can develop into a
chronic condition. Signs and symptoms can vary from mild to severe. Chronic
bacterial conjunctivitis is usually seen in patients with lacrimal duct
obstruction, chronic dacryocystitis, and chronic blepharitis. The most common
caus-ative microorganisms are Streptococcus
pneumoniae, Haemophilusinfluenzae, and
Staphylococcus aureus.
Bacterial
conjunctivitis manifests with an acute onset of red-ness, burning, and
discharge. There is papillary formation, con-junctival irritation, and
injection in the fornices. The exudates are variable but are usually present on
waking in the morning. The eyes may be difficult to open because of adhesions
caused by the exudate. Purulent discharge occurs in severe acute bacterial
in-fections, whereas mucopurulent discharge appears in mild cases. In
gonococcal conjunctivitis, the symptoms are more acute. The exudate is profuse
and purulent, and there is lymphadenopathy. Pseudomembranes may be present.
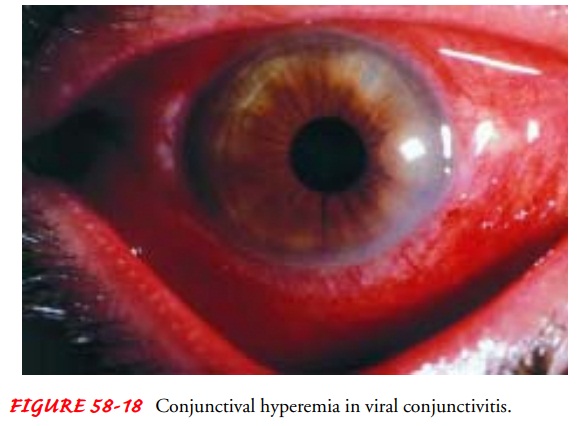
Viral conjunctivitis (Fig. 58-18) can also be acute
and chronic. The discharge is watery, and follicles are prominent. Severe cases
include pseudomembranes. The common causative organisms are adenovirus and
herpes simplex virus. Conjunctivitis caused by adenovirus is highly contagious.
The symptoms include extreme tearing, redness, and foreign body sensation that
can involve one or both eyes. The condition is usually preceded by symptoms of
upper respiratory infection. Corneal involvement causes extreme photophobia.
There is lid edema, ptosis, conjunctival hyperemia
(ie, dilation of the conjunctival blood vessels), watery discharge, follicles,
and papillae. These signs and symptoms vary from mild to severe and may last
for 2 weeks. Viral conjunctivitis, although self-limited, tends to last longer than
bacterial conjunctivitis.

Epidemic
keratoconjunctivitis (EKC) is most often accompa-nied by preauricular
lymphadenopathy and occasionally perior-bital pain. There are marked follicular
and papillary formations. EKC can lead to keratopathy. EKC is a highly
contagious viral conjunctivitis that is easily transmitted from one person to
an-other among household members, school children, and health care workers. The
outbreak of epidemics is seasonal, especially during the summer when people
frequent swimming pools.
Chlamydial conjunctivitis includes trachoma and inclusion conjunctivitis. Trachoma is an ancient disease and is the leading cause of preventable blindness in the world. It is prevalent in areas with hot, dry, and dusty climates and in areas with poor living conditions. It is spread by direct contact or fomites, and the vec-tors can be insects such as flies and gnats.
Trachoma
is a bilateral chronic
follicular conjunctivitis ofchildhood that leads to blindness during adulthood,
if left un-treated. The onset in children is usually insidious, but it can be
acute or subacute in adults. The initial symptoms include red inflamed eyes,
tearing, photophobia, ocular pain, purulent exu-dates, preauricular
lymphadenopathy, and lid edema. Initial oc-ular signs include follicular and
papillary formations. At the middle stage of the disease, there is an acute
inflammation with papillary hypertrophy and follicular necrosis, after which
trichiasis (turning inward of hair follicles) and entropion begin to develop.
The lashes that are turned in rub against the cornea and, after prolonged
irritation, cause corneal erosion and ulceration. The late stage of the disease
is characterized by scarred conjunctiva, subepithelial keratitis, abnormal
vascularization of the cornea (pannus), and residual scars from the follicles
that look like de-pressions in the conjunctiva (ie, Herbert’s pits). Severe
corneal ulceration can lead to perforation and blindness.
Inclusion
conjunctivitis affects sexually active young people who have genital chlamydial
infection. Transmission is by oral-genital sex or hand-to-eye transmission. It
has been reported that indirect transmission has been acquired from
inadequately chlo-rinated swimming pools. The eye lesions usually appear a week
after exposure and may be associated with a nonspecific urethritis or
cervicitis. The discharge is mucopurulent, follicles are present, and there is
lymphadenopathy.
ALLERGIC CONJUNCTIVITIS
Immunologic or allergic conjunctivitis is a hypersensitivity
reac-tion as a part of allergic rhinitis (hay fever), or it can be an
inde-pendent allergic reaction. The patient usually has a history of an allergy
to pollens and other environmental allergens. There is ex-treme itching,
epiphora (ie, excessive secretion of tears), injection, and usually severe
photophobia. The stringlike mucoid discharge is usually associated with rubbing
the eyes because of severe itch-ing. Vernal conjunctivitis is also known as
seasonal conjunctivi-tis because it appears mostly during warm weather. There
may be large formations of papillae that have a cobblestone appearance. It is
more common in children and young adults. Most affected individuals have a
history of asthma or eczema.
TOXIC CONJUNCTIVITIS
Chemical
conjunctivitis can be the result of medications, chlo-rine from swimming pools
(more common during the summer), exposure to toxic fumes among industrial
workers, or exposure to other irritants such as smoke, hair sprays, acids, and
alkalis.
Management
The management of conjunctivitis depends on the
type. Most types of mild and viral conjunctivitis are self-limiting, benign
conditions that may not require treatment and laboratory procedures. For more
severe cases, topical antibiotics, eye drops, or ointment are prescribed.
Patients with gonococcal conjunctivitis require
urgent antibiotic therapy. If left untreated, this ocular disease can lead to
corneal perforation and blindness. The systemic complications can include
meningitis and generalized septicemia.
Acute bacterial conjunctivitis is almost always
self-limiting. If left untreated, the disease follows a 2-week course with
resolution of symptoms. If treated with appropriate antibiotics, it may last
for a few days, with the exception of gonococcal and staphylococcal
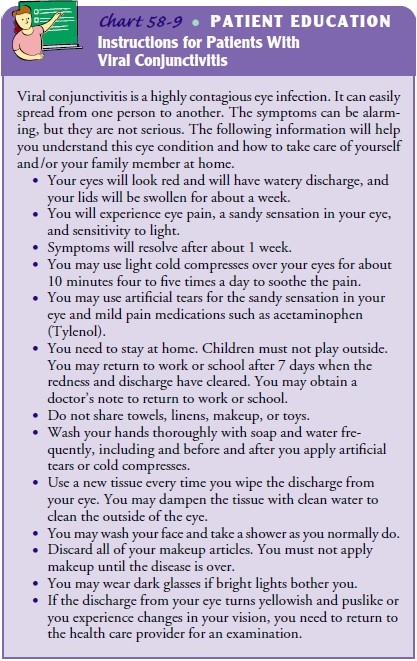
conjunctivitis. Viral conjunctivitis is not responsive to any treatment. Cold
compresses may alleviate some symptoms. It is extremely important to remember
that viral conjunctivitis, especially EKC, is highly transmissible. Patients
must be made aware of the contagious nature of the disease, and adequate
in-structions must be given. These instructions should include an emphasis on
handwashing and avoiding sharing hand towels, face cloths, and eye drops.
Tissues should be directly discarded into a trashcan.
Proper steps must be taken to avoid nosocomial
infections. Frequent hand hygiene, procedures for environmental cleaning, and
disinfection of equipment used for eye examination must be strictly followed at
all times (Chart 58-9). During outbreaks of conjunctivitis caused by
adenovirus, it is necessary that health care facilities assign specified areas
for treating patients with or suspected of having conjunctivitis caused by
adenovirus to pre-vent spread. All forms of tonometry must be avoided unless med-ically
indicated. All multidose medications must be discarded at the end of each day
or when contaminated. Infected employees and others must not be allowed to work
or attend school until symptoms have resolved, which can take 3 to 7 days.
Patients with allergic conjunctivitis, especially recurrent ver-nal or seasonal conjunctivitis, are usually given corticosteroids in ophthalmic preparations. Depending on the severity of the dis-ease, they may be given oral preparations. Use of vasoconstrictors, such as topical epinephrine solution, cold compresses, ice packs, and cool ventilation usually provide comfort by decreasing swelling.
For
trachoma, treatment is usually broad-spectrum antibiotics administered
topically and systemically. Surgical management in-cludes the correction of
trichiasis to prevent conjunctival scarring. Adult inclusion conjunctivitis
requires a 1-week course of anti-biotics. Prevention of reinfection is
important, and affected individuals and their sexual partners must be advised
to seek as-sessment and treatment for sexually transmitted disease, if
indicated.
For conjunctivitis caused by chemical irritants,
the eye must be irrigated immediately and profusely with saline or sterile
water.
Related Topics