Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Eye and Vision Disorders
Assessment of Patients With Eye and Vision Disorders
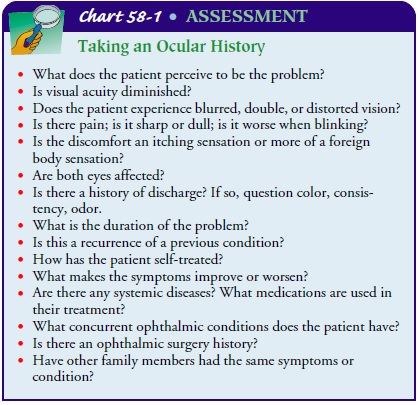
Assessment
The
health care provider, through careful questioning, elicits the necessary
information that can lead to the diagnosis of an oph-thalmic condition.
Pertinent questions to ask during the inter-view can be found in Chart 58-1.
OCULAR EXAMINATION
After
the patient’s chief complaint or concern has been identified and the history
has been obtained, visual acuity should be assessed. This is an essential part
of the eye examination and a measure against which all therapeutic outcomes are
based.
Visual Acuity
Most health care providers are familiar with the
standard Snellen chart. This chart is composed of a series of progressively
smallerrows of letters and is used to test distance vision. The fraction 20/20
is considered the standard of normal vision. Mostpeoplecan see the letters on
the line designated as 20/20 from a distance of 20 feet. A person whose vision
is 20/200 can see an objectfrom
20 feet away that a person whose vision is 20/20 can see from 200 feet away.The patient is positioned at the proscribed distance, usually 20 feet, from the chart and is asked to read the smallest line that he or she can see. The patient should wear distance correction (eyeglasses or contact lenses) if required, and each eye should be tested separately.
The
right eye is commonly tested first and then the left. If the patient is unable
to read the 20/20 line, he or she is given a pinhole occluder and asked to read
again using the eye in question. A makeshift occluder may be created by making
a pinhole in an index card and asking the patient to look through the pinhole.
Squinting produces the same effect. Patients should be encouraged to read more
letters and to guess, if necessary. Often, patients avoid guessing and prefer
not to try at all rather than to make a mistake. The patient should be
encouraged to read every letter possible.
The
visual acuity (VA) is recorded in the following way. If the patient reads all
five letters from the 20/20 line with the right eye (OD) and three of the five
letters on the 20/15 line with the left eye (OS), the examiner writes OD 20/20,
OS 20/15-2, or VA 20/20, 20/15-2.
If the patient is unable to read the largest letter
on the chart (the 20/200 line), the patient should be moved toward the chart or
the chart moved toward the patient, until the patient is able to identify the
largest letter on the chart. If the patient can recognize only the letter E on
the top line at a distance of 10 feet, the visual acuity would be recorded as
10′/200. If the patient is unable to see the letter E at any
distance, the examiner should determine if the patient can count fingers (CF).
The examiner holds up a ran-dom number of fingers and asks the patient to count
the number he or she sees. If the patient correctly identifies the number of
fin-gers at 3 feet, the examiner would record CF/3′.
If
the patient is unable to count fingers, the examiner raises one hand up and
down or moves it side to side and asks in which direction the hand is moving.
This level of vision is known as hand motions (HM). A patient who can perceive
only light is de-scribed as having light perception (LP). The vision of a
patient who is unable to perceive light is described as no light perception
(NLP).
The External Eye Examination
After
the visual acuity has been recorded, an external eye exami-nation is performed.
The position of the eyelids is noted. Com-monly, the upper 2 mm of the iris is
covered by the upper lid. The patient is examined for ptosis (ie, drooping eyelid) and for lid retraction (ie, too much
of the eye exposed). Sometimes, the upper or lower lid turns out, affecting
closure. The lid margins and lashes should have no edema, erythema, or lesions.
The ex-aminer looks for scaling or crusting, and the sclera is inspected. A
normal sclera is opaque and white. Lesions on the conjunctiva, discharge, and
tearing or blinking are noted.
The
room should be darkened so that the pupils can be ex-amined. The pupillary
response should be checked with a pen-light to be certain that the pupils are
equally reactive and regular. A normal pupil is black. An irregular pupil may
result from trauma, previous surgery, or a disease process.
The
patient’s eyes are observed in primary or direct gaze, and any head tilt is
noted. A tilt may indicate cranial nerve palsy. The patient is asked to stare
at a target; each eye is covered and un-covered quickly while the examiner
looks for any shift in gaze. The examiner observes for nystagmus (ie, oscillating movement of the eyeball). The extraocular
movements of the eyes are sim-ply tested by having the patient follow the
examiner’s finger or hand light through the six cardinal directions of gaze
(ie, up, down, right, left, and both diagonals). This is especially impor-tant
when screening patients for ocular trauma or for neurologic disorders.
Related Topics