Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Eye and Vision Disorders
Impaired Vision: Refractive Errors, Low Vision and Blindness
Impaired Vision
REFRACTIVE ERRORS
In refractive errors, vision is impaired because a
shortened or elongated eyeball prevents light rays from focusing sharply on the
retina. Blurred vision from refractive error can be corrected with eyeglasses
or contact lenses. The appropriate eyeglass or contact lens is determined by refraction. Refraction ophthalmology
con-sists of placing various types of lenses in front of the patient’s eyes to
determine which lens best improves the patient’s vision.
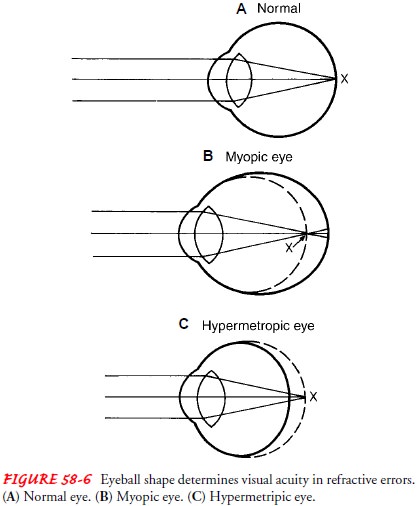
The depth of the eyeball is important in
determining refractive error (Fig. 58-6). Patients for whom the visual image
focuses pre-cisely on the macula and who do not need eyeglasses or contact
lenses are said to have emmetropia
(normal vision). People who have myopia
are said to be nearsighted. They have deeper eye-balls; the distant visual
image focuses in front of, or short of, the retina. Myopic people experience
blurred distance vision. When people have a shorter depth to their eyes, the
visual image focuses beyond the retina; the eyes are shallower and are called
hyperopic. People with hyperopia are
farsighted. These patients experience near vision blurriness, whereas their
distance vision is excellent.
Another important cause of refractive error is astigmatism, an irregularity in the curve of the cornea. Because astigmatism causes a distortion of the visual image, acuity of distance and near vision can be decreased. Eyeglasses with a cylinder correction or rigid or soft toric contact lenses are appropriate for these patients.
LOW VISION AND BLINDNESS
Low
vision is a general term
describing visual impairment that re-quires patients to use devices and
strategies in addition to correc-tive lenses to perform visual tasks. Low
vision is defined as a best corrected visual acuity (BCVA) of 20/70 to 20/200
(Table 58-1).
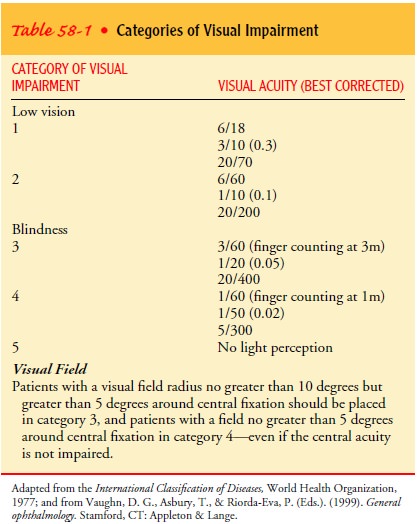
Blindness is
defined as a BCVA of 20/400 to no light per-ception. The clinical definition of
absolute blindness is the ab-sence of light perception. Legal blindness is a
condition of impaired vision in which an individual has a BCVA that does not
exceed 20/200 in the better eye or whose widest visual field di-ameter is 20
degrees or less. This definition does not equate with functional ability, nor
does it classify the degrees of visual im-pairment. Legal blindness ranges from
an inability to perceive light to having some vision remaining. An individual
who meets the criteria for legal blindness may obtain government financial
assistance. There are more than 1,046,000 legally blind Ameri-cans who are 40
years of age or older. African Americans have a higher rate of blindness than
do Caucasians (Preshel & Prevent Blindness America, 2002).
Impaired vision is accompanied by difficulty in performing functional activities. Individuals with visual acuity of 20/80 to 20/100 with a visual field restriction of 60 degrees to greater than 20 degrees can read at a nearly normal level with optical aids. Their visual orientation is near normal but requires increased scanning of the environment (ie, systematic use of head and eye movements). In a visual acuity range of 20/200 to 20/400 with a 20-degree to greater than 10-degree visual field restriction, the individual can read slowly with optical aids.
His or her visual orientation
is slow, with constant scanning of the environment; individuals in this
category have travel vision. Individuals with hand motion vision or no vision
may benefit from the use of mo-bility devices (eg, cane, guide dog) and should
be encouraged to learn Braille and to use computer aids.
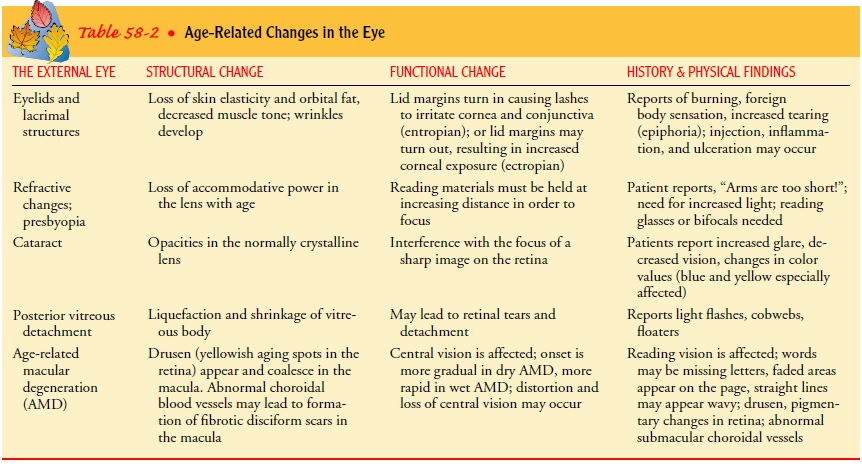
The
most common causes of blindness and visual impairment among adults 40 years of
age or older are diabetic retinopathy, macular degeneration, glaucoma, and
cataracts, (Preshel & Pre-vent Blindness America, 2002). Macular
degeneration is more prevalent among Caucasians, whereas glaucoma is more
preva-lent among African Americans. Age-related changes in the eye are
described in Table 58-2.
Low-Vision Assessment
The assessment of low vision includes a thorough
history and the examination of distance and near visual acuity, visual field,
contrast sensitivity, glare, color perception, and refraction. Specially
de-signed, low-vision visual acuity charts are used to evaluate patients.
PATIENT INTERVIEW
During history taking, the cause and duration of
the patient’s vi-sual impairment are identified. Patients with retinitis
pigmentosa, for example, have a genetic abnormality. Patients with diabetic macular
edema typically have fluctuating visual acuity. Patients with macular
degeneration have central acuity problems. Central acuity problems cause
difficulty in performing activities that re-quire finer vision, such as
reading. People with peripheral field defects have more difficulties with
mobility. The patient’s cus-tomary activities of daily living, medication
regimen, habits (eg, smoking), acceptance of the physical limitations brought
about by the visual impairment, and realistic expectations of low-vision aids
must also be identified. These aspects of the patient’s activi-ties are
important indicators for planning care that will include guidelines for safety
and referrals to social services.
ASSESSMENT
Contrast-sensitivity
testing measures visual acuity in different de-grees of contrast. The initial
test may take the form of simply turning on the lights while testing the
distance acuity. If the pa-tient can read better with the lights on, the
patient can benefit from magnification. Glare testing enables the examiner to
obtain a more realistic evaluation of the patient’s ability to function in his
or her environment. Glare can reduce a person’s ability to see, especially in
patients with cataracts. Devices that test glare, such as the Brightness Acuity
Tester, produce three degrees of bright light to create a dazzle effect while
the patient is viewing a target, such as Snellen letters on the wall. The
lights have been calibrated to imitate certain objects that create glare, such
as the brightness of a car’s headlights at night.
Medical Management
Managing low vision involves magnification and
image enhance-ment through the use of low-vision aids and strategies and
through referrals to social services and community agencies serv-ing the
visually impaired. The goals are to enhance visual func-tion and assist
patients with low vision to perform customary activities. Low-vision aids
include optical and nonoptical devices (Table 58-3). The optical devices
include convex lens aids, such as magnifiers and spectacles; telescopic
devices; anti-reflective lenses that diminish glare; and electronic reading
systems, such as closed-circuit television and computers with large print.
Contin-uing advances in computer software provide very useful products for
patients with low vision. Scanners teamed with the appro-priate software enable
the user to scan printed data into the computer and have it read by computer
voice or to increase the magnification for reading. Magnifiers can be hand-held
or at-tached to a stand with or without illumination. Telescopic de-vices can
be spectacle telescopes or clip-on or hand-held loupes.
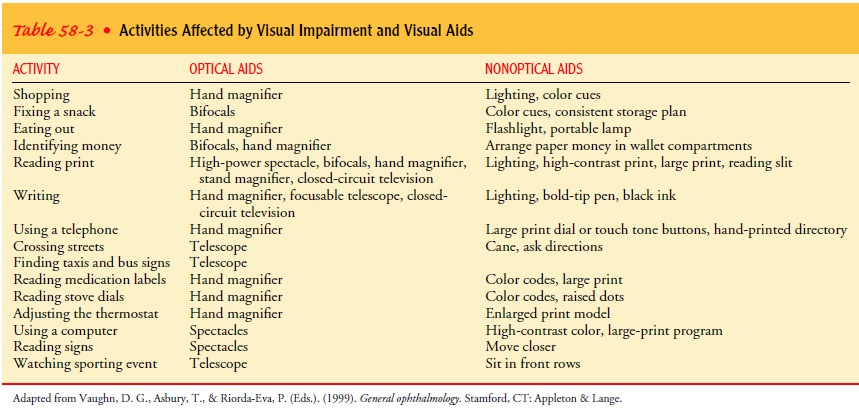
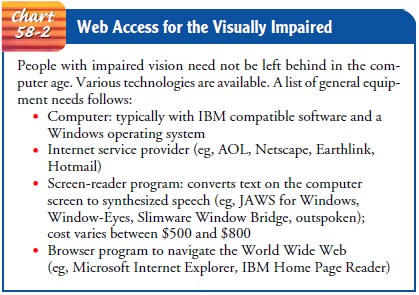
Nonoptical aids include large-print publications and a variety of writing aids. The Internet continues to expand, and a tele phone system has been developed that allows access to the Inter-net and e-mail using voice commands (see Chart 58-2).
Strategies that enhance the performance of visual tasks in-clude modification of body movements and illumination and training for independent living skills. Head movements and positions can be modified to place images in functional areas of the visual field. Illumination is an added feature in magnifiers. Adjusting the lighting helps with reading and other activities. Simple optical and nonoptical aids are available in low-vision clinics.
Referrals
to community agencies may be necessary for low-vision patients living alone who
are unable to self-administer their medications. Community agencies, such as
The Lighthouse National Center for Vision and Aging, offer services to
low-vision patients that include training in independent living skills and the
provision of occupational and recreational activities and a wide variety of
assistive devices for vision enhancement and orienta-tion and mobility.
VISION RESTORATION FOR THE BLIND
Ophthalmologists
have worked toward visual restoration for blind individuals for years, and
computer technology now pro-vides opportunities for restoring sight. For
example, a multiple-unit artificial retina chipset (MARC) has been devised for
implanting within the eye. The MARC can be enabled to receive signals from an
external camera mounted in a glasses frame. The acquired image is wirelessly
transmitted to the chip, which pro-vides a type of artificial vision and which,
with training, allows the patient to achieve some useful vision. Although the
device is still experimental, some work has been done with patients who have
lost vision from retinitis pigmentosa and age-related macu-lar degeneration
(Humayan et al., 1999).
Nursing Management
Coping
with blindness involves three types of adaptation: emo-tional, physical, and
social. The emotional adjustment to blind-ness or severe visual impairment
determines the success of the physical and social adjustments of the patient.
Successful emo-tional adjustment means acceptance of blindness or severe visual
impairment.
PROMOTING COPING EFFORTS
Effective coping may not occur until the patient
recognizes the permanence of the blindness. Clinging to false hopes of
regain-ing vision hampers effective adaptation to blindness. A newly blind
patient and his or her family members (especially those who live with the
patient) undergo the various steps of grieving: de-nial and shock, anger and
protest, restitution, loss resolution, and acceptance. The ability to accept
the changes that must come with visual loss and willingness to adapt to those
changes influence the successful rehabilitation of the patient who is blind.
Additional aspects to consider are value changes, independence–dependence
conflicts, coping with stigma, and learning to function in social settings
without visual cues and landmarks.
PROMOTING SPATIAL ORIENTATION AND MOBILITY
People
who are blind detect and incorporate less information about their environment
than do sighted people. The blind per-son relies on egocentric, sequential, and
positional information, which centers on the person and his or her relationship
to the ob-jects in the environment. For example, the topographic concepts of
front, back, left, right, above, and below and measures of dis-tances are most
useful in determining the exact position, se-quence, and location of objects in
relation to the person who is blind. Although their basis of information may be
different from that of sighted people, people who are blind can comprehend
spa-tial concepts.
The goal of orientation and mobility training is to
foster in-dependence in the environment. Training may be accomplished by using
auditory and tactile cues and by providing anticipatory information. Having a
concept of the spatial composition of the environment (ie, cognitive map)
enhances independence of those who are blind. Orientation and mobility training
programs are offered by community agencies serving the blind or visually
im-paired. Training includes using mobility devices for travel, the long cane,
electronic travel aids, dog guides, and orientation aids. The basic orientation
and mobility techniques used by a sighted person to assist a person who is
blind or visually impaired to am-bulate safely and efficiently are called
sighted-guide techniques.
Spatial Orientation and
Mobility in Institutional Settings.A blindor severely visually impaired patient requires strategies for
adapt-ing to the environment. The monocular postoperative patient whose
functioning eye is restricted by a surgical patch or by post-operative
inflammation requires early ambulation just like any postoperative patient. The
activities of daily living, such as walking to a chair from a bed, require
spatial concepts. The patient needs to know where he or she is in relation to
the rest of the room, to understand the changes that may occur, and how to
approach the desired location safely. This requires a collaborative effort
be-tween the patient and the nurse, who serves as the sighted guide.
Patients
whose visual impairment results from a chronic pro-gressive eye disorder, such
as glaucoma, have better cognitive mapping skills than the suddenly blinded
patient. They have de-veloped the use of spatial and topographic concepts early
and gradually; hence, remembering a room layout is easier for them. Suddenly
blinded patients have more difficulty in adjusting; and emotional and
behavioral issues of coping with blindness may hinder their learning. These
patients require intensive emotional support. The nurse must assess the degree
of physical assistance the patient with a visual deficit requires and
communicate this to other health care personnel.
The food tray’s composition is likened to the face
of a clock. For example, the main plate may be described as being at 12 o’clock
or the coffee cup at 3 o’clock. In the hospital, the bedside table and the call
button must always be within reach. The parts of the call button are explained,
and the patient is encouraged to touch and press the buttons or dials until the
activity is mastered. The patient must be familiarized with the location of the
telephone, water pitcher, and other objects on the bedside table. All articles
and furniture must be replaced in the same positions. Introducing oneself on
entering a patient’s room is always a polite gesture and helps in the
orientation of a blind patient.
The nurse should be aware of the importance of
technique in providing physical assistance, developing independence, and
en-suring safety. The readiness of the patient and his or her family to learn
must be assessed before initiating orientation and mobil-ity training.
Teaching Patients Self-Care.The nurse, social workers,
family,and others collaborate to assess the patient’s home condition and
support system. If available, a low-vision specialist should be con-sulted
before discharge, particularly for patients for whom iden-tifying and
administering medications pose problems. The level of visual acuity and patient
preference help to determine appro-priate interventions. For example, a plastic
pill container with di-viders that has been prefilled with a week’s supply of
medication can make medication administration easier for some patients, whereas
others may prefer to have medication bottles marked with textured paints. Many
patients require referral to social ser-vices. Patients with habits that may
jeopardize safety, such as smoking, need to be cautioned and assisted to make
their envi-ronment safe.
Community Programs and
Services.In the United States,
lawssuch as the Rehabilitation Act, the Civil Rights Act, and the Americans
With Disabilities Act support assistance of the blind. Governmental services
include income assistance through Social Security Disability Income and
Supplemental Security Income; health insurance through Medicaid and Medicare
programs; support services, such as vocational rehabilitation programs of-fered
by the Division of Blind Services; tax exemptions and tax deductions;
Department of Veterans Affairs programs for visually impaired veterans; and
U.S. Postal Service reduced postage for Braille materials and talking books.
Related Topics