Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Eye and Vision Disorders
Retinal Detachment - Retinal Disorders
Retinal Disorders
Although the retina is composed of multiple
microscopic layers, the two innermost layers, the sensory retina and the
retinal pig-ment epithelium (RPE), are the most relevant to common retinal
disorders. Just as the film in a camera captures an image, so does the retina,
the neural tissue of the eye. The rods and cones, the photoreceptor cells, are
found in the sensory layer of the retina. Beneath the sensory layer lies the
RPE, the pigmented layer. When the rods and cones are stimulated by light, an
electrical impulse is generated, and the image is transmitted to the brain.
RETINAL DETACHMENT
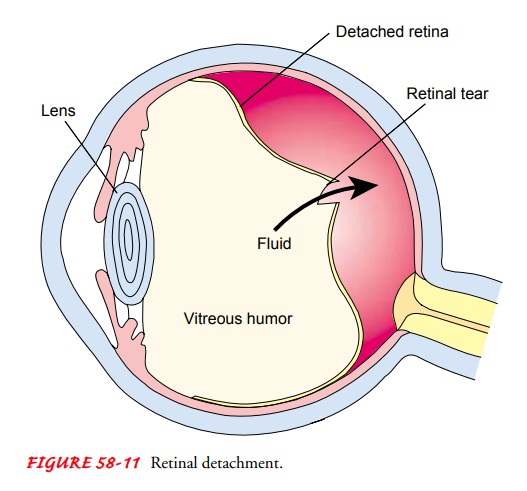
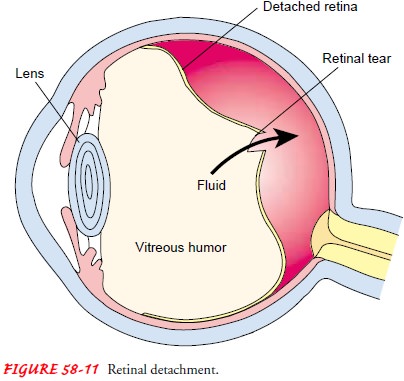
Retinal
detachment refers to the separation of the RPE from the sensory layer. The four
types of retinal detachment are rheg-matogenous, traction, a combination of
rhegmatogenous and traction, and exudative. Rhegmatogenous
detachment is the most common form. In this condition, a hole or tear
develops in the sen-sory retina, allowing some of the liquid vitreous to seep
through the sensory retina and detach it from the RPE (Fig. 58-11). People at
risk for this type of detachment include those with high myopia or aphakia after cataract surgery. Trauma
may also play a role in rhegmatogenous retinal detachment. Between 5% and 10%
of all rhegmatogenous retinal detachments are associated with proliferative
retinopathy, a retinopathy associated with dia-betic neovascularization.
Tension,
or a pulling force, is responsible for traction
retinaldetachment. An ophthalmologist must ascertain all of the areas
ofretinal break and identify and release the scars or bands of fibrous material
providing traction on the retina. Generally, patients with this condition have
developed fibrous scar tissue from conditions such as diabetic retinopathy,
vitreous hemorrhage, or the retinopa-thy of prematurity. The hemorrhages and
fibrous proliferation as-sociated with these conditions exert a pulling force
on the delicate retina.
Patients
can have both rhegmatogenous and traction retinal detachment. Exudative retinal detachments are the
result of the production of a serous fluid under the retina from the choroid.
Conditions such as uveitis and macular degeneration may cause the production of
this serous fluid.
Clinical Manifestations
Patients
may report the sensation of a shade or curtain coming across the vision of one
eye, cobwebs, bright flashing lights, or the sudden onset of a great number of
floaters. Patients do not com-plain of pain.
Assessment and Diagnostic Findings
After visual acuity is determined, the patient must have a dilated fundus examination using an indirect ophthalmoscope and a Goldmann three-mirror examination. This examination is detailed and prolonged, and it can be very uncomfortable for the patient. Many patients describe this as looking directly into the sun. All retinal breaks, all fibrous bands that may be causing traction on the retina, and all degenerative changes must be identified. A de-tailed retinal drawing is made by the ophthalmologist.
Surgical Management
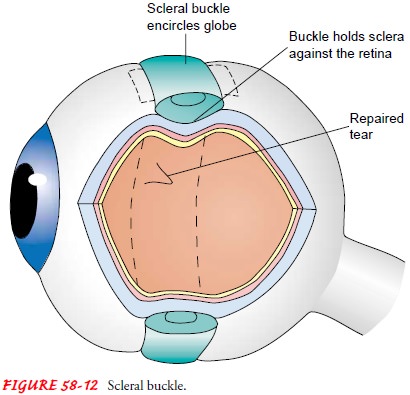
In
rhegmatogenous detachment, an attempt is made to reattach the sensory retina to
the RPE surgically. The retinal surgeon com-presses the sclera (often with a
scleral buckle or a silicone band; Fig. 58-12) to indent the scleral wall from
the outside of the eye and bring the two retinal layers in contact with each
other. Gas bubbles, silicone oil, or perfluorocarbon and liquids may also be
injected into the vitreous cavity to help push the sensory retina up against
the RPE. Argon laser photocoagulation or cryotherapy is also used to
“spot-weld” small holes.
In traction retinal detachment, a vitrectomy is
performed. A vit-rectomy is an intraocular procedure in which 1- to 4-mm
incisions are made at the pans plana. One incision allows the introduction of a
light source (ie, endoilluminator), and another incision serves as the portal
for the vitrectomy instrument. The surgeon dissects preretinal membranes under
direct visualization while the retina is stabilized by an intraoperative
vitreous substitute. Technologic advances, including the use of operating
microscopes, micro-instrumentation, irrigating contact lenses, and instruments
that combine vitreous cutting, aspiration, and illumination capabili-ties into
one device, have allowed tremendous progress in vitre-oretinal surgery. The
techniques of vitreoretinal surgery can be used in various procedures,
including the removal of foreign bodies, vitreous opacities such as blood, and
dislocated lenses. Traction on the retina may be relieved through vitrectomy
and may be combined with scleral buckling to repair retinal breaks. Treatment
of macular holes includes vitrectomy, laser photo-coagulation, air-fluid-gas
exchanges, and the use of growth factor.
Nursing Management
For the most part, nursing interventions consist of educating the patient and providing supportive care.
PROMOTING COMFORT
If
gas tamponade is used to flatten the retina, the patient may have to be
specially positioned to make the gas bubble float into the best position. Some
patients must lie face down or on their side for days. Patients and family
members should be made aware of these special needs beforehand, so that the
patient can be made as comfortable as possible.
TEACHING ABOUT COMPLICATIONS
In many cases, vitreoretinal procedures are
performed on an out-patient basis, and the patient is seen the next day for a
follow-up examination and closely monitored thereafter as required.
Post-operative complications in these patients may include increased IOP,
endophthalmitis, development of other retinal detach-ments, development of
cataracts, and loss of turgor of the eye. Pa-tients must be taught the signs
and symptoms of complications, particularly of increasing IOP and postoperative
infection.
Related Topics